Imagine a scenario where a road is blocked, causing a traffic jam and preventing cars from reaching their destinations smoothly.
Similarly, sinus infections can create a blockage in the nasal passages, affecting the delicate connection between the nose and ears.
This interference can lead to issues with hearing, making it vital to understand how sinusitis can impact our auditory health.
As we explore the intricate relationship between sinus infections and hearing loss, we uncover essential insights that shed light on effective prevention and treatment strategies for maintaining optimal hearing function.
Key Takeaways
- Sinus infections can lead to fluid buildup and Eustachian tube dysfunction, affecting hearing.
- Symptoms like ear pressure, muffled sounds, and temporary hearing loss indicate sinus-related issues.
- Treatment options include antibiotics, decongestants, and nasal sprays to alleviate symptoms.
- Timely management and proactive measures are crucial to prevent and address sinus-induced hearing problems.
Understanding Sinus Infections and Hearing Loss
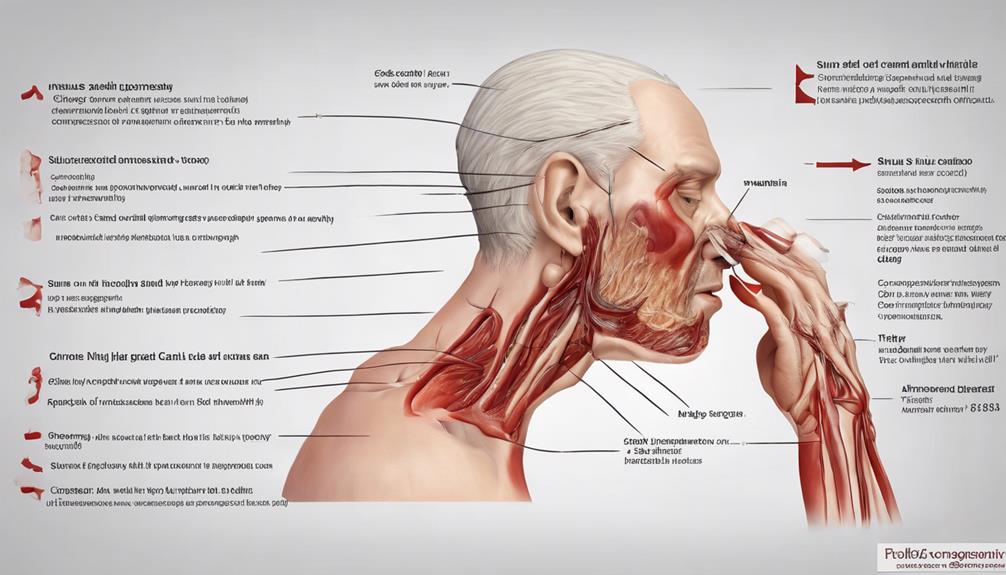
When sinus infections occur, they can impact hearing by causing fluid buildup in the ear, predominantly affecting the Eustachian tube. This fluid accumulation can disrupt the normal functioning of the ear, leading to symptoms such as muffled hearing, ear pressure, and even temporary hearing loss.
The sinuses and ears are intricately connected through the Eustachian tube, which helps regulate air pressure in the middle ear. When the sinuses become inflamed due to an infection, this inflammation can extend to the Eustachian tube, causing it to swell and become blocked.
As a result, the normal drainage of fluid from the middle ear is impaired, leading to a buildup of fluid and pressure. This pressure can impact the ability of the ear to transmit sound properly, resulting in hearing difficulties. Understanding the relationship between sinus infections and hearing loss is crucial in managing these conditions effectively and preserving ear health.
Mechanisms of Sinus-Related Hearing Loss
In cases of sinus-related hearing loss, inflammation in the nasal cavity and sinuses can disrupt the Eustachian tube and middle ear, leading to potential fluid accumulation and pressure variations that impact auditory function.
Mechanisms of Sinus-Related Hearing Loss:
- Eustachian Tube Dysfunction: Inflammation can cause the Eustachian tube to swell and become blocked, hindering proper ventilation and drainage in the middle ear.
- Middle Ear Fluid Accumulation: Blocked Eustachian tubes can result in the accumulation of fluid in the middle ear, leading to conductive hearing loss.
- Cochlear Effects: Chronic sinusitis can contribute to sensorineural hearing loss by affecting cochlear functions, particularly the delicate outer hair cells crucial for sound signal transmission.
- Correlation with Chronic Rhinosinusitis (CRS): Studies have indicated a relationship between the severity of CRS and the presence of sensorineural hearing loss, highlighting the interconnectedness of sinus health and auditory function.
Understanding these mechanisms can shed light on how sinus issues can impact hearing and the importance of managing sinusitis to preserve auditory health.
Symptoms of Sinusitis-Induced Hearing Issues
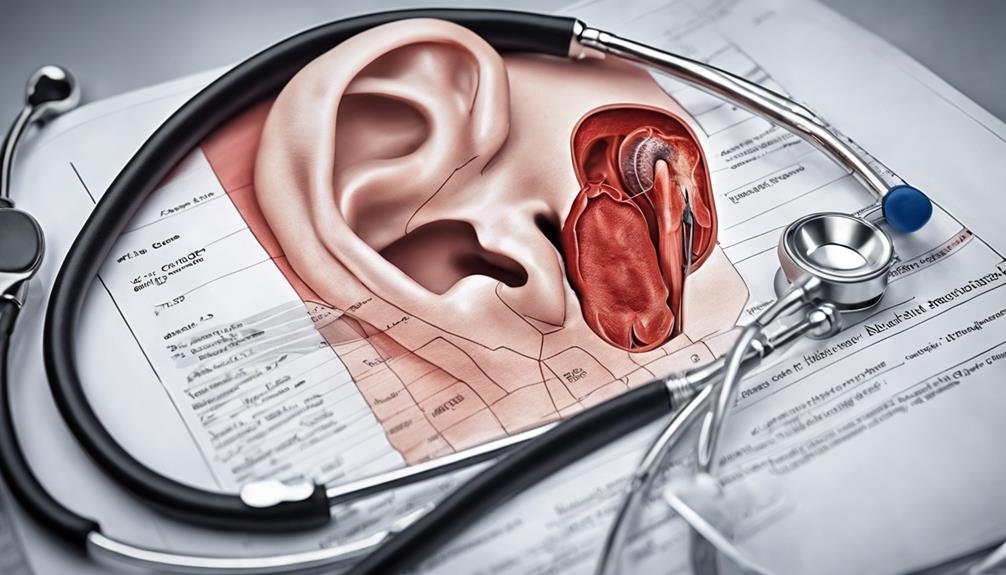
Symptoms commonly associated with sinusitis-induced hearing issues encompass ear pressure, muffled sounds, and difficulties in clear hearing, often accompanied by ear pain, tinnitus, and vertigo.
When sinus infections occur, they can lead to inflammation and blockages that affect the Eustachian tube, which is responsible for equalizing pressure in the ear. This blockage can cause a feeling of fullness or pressure in the ear, making sounds seem muffled or distant. Additionally, the accumulation of fluid in the ear due to sinus blockage can result in temporary hearing loss.
Ear pain is a frequent complaint in individuals experiencing sinus-related hearing problems, as the pressure changes within the ear can cause discomfort. Tinnitus, characterized by ringing or buzzing sounds in the ear, is another common symptom that may accompany sinusitis-induced hearing issues.
Furthermore, vertigo, a sensation of dizziness or spinning, can also manifest in individuals with sinus infections affecting their hearing. Understanding these symptoms can prompt timely intervention for individuals facing sinus-related ear disturbances.
Treatment Options for Sinus Infection-Related Hearing Loss

Experiencing sinus infection-related hearing loss necessitates exploring diverse treatment options aimed at alleviating symptoms and restoring auditory function. Here are key approaches that can help address sinus infection-related hearing issues:
- Antibiotics: Prescribed to treat bacterial infections causing sinusitis, helping to clear up the underlying infection and reduce inflammation in the sinuses that may be impacting hearing.
- Decongestants: These medications can help reduce nasal congestion, open up the Eustachian tube, and relieve pressure in the ears, improving hearing abilities.
- Saline Nasal Sprays: Useful for clearing out mucus and reducing inflammation in the sinuses, potentially alleviating ear-related symptoms and improving overall comfort.
- Antihistamines: Sometimes utilized to manage allergies contributing to sinusitis, these medications can help alleviate associated ear discomfort and improve hearing quality.
These treatment options, when used appropriately under medical guidance, can play a crucial role in addressing sinus infection-related hearing loss and promoting better auditory health.
Preventing Hearing Complications From Sinus Infections
To effectively prevent hearing complications stemming from sinus infections, timely treatment and proactive management are essential. Addressing sinus congestion and inflammation promptly can help reduce the risk of Eustachian tube blockage, which can lead to temporary hearing loss.
Seeking medical assistance for persistent sinus pressure and hearing problems is crucial in preventing long-term damage to the ears. Effective management of sinus infections through medications and interventions can safeguard against sinus-related hearing complications.
Regular monitoring and treatment by ENT specialists play a significant role in mitigating the impact of sinus infections on hearing health. By staying vigilant about sinus health and seeking appropriate medical care when needed, individuals can take proactive steps to prevent potential hearing issues associated with sinus infections.
Frequently Asked Questions
Can Sinus Infections Lead to Permanent Hearing Loss?
Yes, sinus infections can lead to permanent hearing loss if left untreated. Prolonged sinusitis may damage middle ear structures, causing lasting hearing impairment.
Fluid buildup from chronic sinusitis can harm the hearing mechanism irreversibly. Prompt treatment can prevent progression to permanent hearing loss.
Managing sinus-related hearing issues promptly is vital for preserving hearing function.
How Can I Regain Hearing After a Sinus Infection?
We must address hearing loss post-sinus infection promptly. Seeking treatment like antibiotics, antihistamines, and decongestants can aid in recovery. Consider minimally invasive procedures such as balloon sinuplasty for sinus-related hearing issues.
Consulting with an ENT specialist early on is crucial for regaining lost hearing. Regular monitoring of sinus and ear health is key to preventing long-term complications. Take proactive steps to restore your hearing after a sinus infection.
How Do You Unblock Your Ears From a Sinus Infection?
To unblock our ears from a sinus infection, we can try using a saline nasal spray to clear congestion and reduce pressure.
The Valsalva maneuver, where we gently blow through our nose while pinching it closed, can help equalize ear pressure.
Steam inhalation with a towel over our head can open up sinuses and ears, while chewing gum or yawning can relieve ear pressure from sinus congestion.
If the blockage persists, consulting a healthcare provider is recommended.
How Long Does It Take for Ears to Clear After Sinus Infection?
We've experienced that ears typically clear up within a few days to weeks after a sinus infection. The time for this clearance varies based on each person's immune response and the severity of the infection.
Occasionally, some may still feel pressure or mild hearing issues in the ears even after sinusitis treatment. Proper management and follow-up care for sinus infections can help speed up the ear-clearing process.
Conclusion
In conclusion, sinus infections can indeed lead to hearing loss through the obstruction of the Eustachian tube. By understanding the mechanisms behind this link, recognizing the symptoms, seeking appropriate treatment, and taking preventive measures, individuals can protect their hearing from the potential complications of sinusitis.
Remember, knowledge is power in preserving your auditory health. Stay informed, stay proactive, and safeguard your ears from the impact of sinus infections.