Cortical auditory evoked potentials (CAEPs) are widely used in clinics to assess hearing and auditory processing. They help detect hearing issues in newborns, monitor children’s auditory development, and evaluate how well cochlear implants work. CAEPs also assist in diagnosing neurological conditions affecting hearing and guiding hearing aid adjustments. If you stay tuned, you’ll discover how these responses support early diagnosis, tailored interventions, and understanding brain plasticity related to sound processing.
Key Takeaways
- Assess hearing and neural pathway integrity in newborns, infants, and challenging populations for early diagnosis.
- Detect auditory processing disorders in children to guide targeted interventions using electrophysiological markers.
- Monitor cochlear implant effectiveness and neural adaptation through cortical response tracking over time.
- Aid in differential diagnosis of peripheral versus central auditory disorders by analyzing cortical response patterns.
- Support prognosis and treatment planning by evaluating neural plasticity, recovery potential, and progression of neurological conditions.
Assessing Hearing in Newborns and Infants

Evaluating hearing in newborns and infants is essential for early detection of auditory impairments, which can particularly influence language development. Cortical auditory evoked potentials help assess neural timing, providing insight into how well auditory pathways are functioning. These tests measure the brain’s response to sounds, revealing the integrity of neural signals traveling from the ear to the auditory cortex. When neural timing is delayed or abnormal, it indicates potential issues in the auditory pathways that could affect speech and language acquisition. This assessment allows clinicians to identify hearing concerns early, even before behavioral signs appear. By understanding the efficiency of auditory pathways during this critical period, you can intervene promptly, supporting better developmental outcomes for the child. Additionally, advancements in automation technology are enhancing the precision and speed of these diagnostic assessments, facilitating earlier and more accurate detection of auditory processing issues.
Detecting Auditory Processing Disorders in Children

You can use electrophysiological markers to detect auditory processing disorders in children accurately. These objective diagnosis strategies help identify issues that might not be evident through behavioral tests alone. Understanding these tools allows you to assess auditory function efficiently and plan appropriate interventions.
Electrophysiological Markers Identification
Electrophysiological markers serve as essential tools for detecting auditory processing disorders (APDs) in children, offering objective insights into how their brains respond to sounds. Neural markers, such as specific cortical responses, help identify atypical auditory processing patterns. These diagnostic indicators reveal differences in the timing, amplitude, and morphology of auditory evoked potentials, which reflect how efficiently a child’s brain processes sound information. By analyzing these markers, you can distinguish between typical and abnormal auditory processing, often before behavioral symptoms become evident. Accurate identification of neural markers supports early intervention, guiding targeted therapies to improve auditory skills. Additionally, understanding the contrast ratio of auditory responses enhances the precision of diagnosis. Overall, electrophysiological markers provide a reliable, non-invasive means to detect APDs, enabling timely and effective clinical decision-making.
Objective Diagnosis Strategies
Objective diagnosis strategies for detecting auditory processing disorders in children rely on non-invasive, neurophysiological assessments that provide direct insights into the brain’s response to sound. Cortical auditory evoked potentials (CAEPs) reveal how neural pathways process auditory stimuli, making them essential for identifying deficits. These assessments also reflect neural plasticity, showing how the brain adapts or reorganizes in response to auditory challenges. Cortical reorganization, often seen in children with processing issues, can be detected through changes in CAEP patterns. By analyzing these responses, clinicians can pinpoint where processing may be disrupted. This approach enables early diagnosis, guiding targeted interventions that leverage the brain’s capacity for plasticity to improve auditory function.
Monitoring Auditory Function in Cochlear Implant Users
Monitoring neural activation helps you track how well the cochlear implant stimulates the auditory pathway. By evaluating this activity, you can evaluate whether the implant is effectively supporting auditory function. This process is essential for determining implant efficacy and optimizing patient outcomes. Incorporating filter replacement indicators into your assessment can help ensure the device continues to perform optimally over time.
Monitoring Neural Activation
Tracking neural activation in cochlear implant users is essential for evaluating how well the device stimulates the auditory nerve. By monitoring cortical responses, you can assess auditory attention, revealing how effectively users focus on sounds. Changes in cortical activity also indicate cortical plasticity, showing how the brain adapts to the implant over time. Cortical auditory evoked potentials help identify whether the neural pathways are being properly activated, providing real-time feedback on neural engagement. This information guides adjustments to the implant settings, ensuring ideal stimulation. You can observe patterns of activation that reflect the user’s ability to attend to auditory stimuli and adapt to their environment. Monitoring neural activation thus supports personalized interventions and improved long-term outcomes for cochlear implant users. Understanding tableware highlights how cultural and material factors influence design and functionality, similar to how neural responses reveal functional adaptations in auditory processing.
Assessing Implant Efficacy
Evaluating implant efficacy involves examining how well a cochlear implant restores auditory function and enables you to perceive sounds accurately. Cortical auditory evoked potentials reveal neural synchronization between the implant and the auditory cortex, indicating effective signal transmission. Improved neural synchronization suggests that your brain is processing sounds more precisely. Additionally, cortical plasticity plays a fundamental role in adapting to the implant over time, enhancing speech understanding and sound discrimination. By monitoring cortical responses, you can assess how well your auditory system is adapting and whether the implant’s stimulation is effective. These measurements help clinicians optimize programming settings, track progress, and determine if additional training or intervention is needed to maximize auditory performance. Regular assessment of credit card security measures can also help in safeguarding patient data during clinical processes.
Evaluating Neurological Conditions Affecting Hearing

Evaluating neurological conditions that impact hearing often involves analyzing cortical auditory evoked potentials (CAEPs), which reflect brain responses to sound stimuli. CAEPs help detect abnormal neural activity, assess auditory pathway integrity, and monitor cortical reorganization due to injury or disease. Changes in CAEP patterns can indicate neural plasticity, where the brain adapts to damage by reorganizing auditory processing areas. This insight guides diagnosis and intervention strategies. Enhanced natural language processing in CAEP analysis can improve the interpretation of complex neural responses. The table below summarizes key aspects:
| Condition | CAEP Findings | Clinical Implication |
|---|---|---|
| Auditory cortex lesions | Absent or delayed responses | Identifies cortical damage |
| Neural reorganization | Altered amplitude/latencies | Indicates cortical reorganization |
| Multiple sclerosis | Prolonged latencies | Reflects demyelination affecting hearing |
Understanding these patterns helps tailor treatments and track recovery.
Objective Hearing Screening in Difficult-to-Test Populations

When evaluating hearing in populations who cannot reliably participate in traditional behavioral tests—such as infants, individuals with developmental disabilities, or neurological conditions—objective screening methods become indispensable. Cortical auditory evoked potentials provide a non-invasive way to assess auditory pathway integrity without requiring active cooperation. These tools capitalize on neural plasticity, recognizing that cortical responses can adapt through cortical reorganization, especially after hearing loss or auditory deprivation. By measuring cortical activity directly, you can detect hearing impairments early, facilitating timely intervention. This approach ensures accurate screening even in challenging populations, reducing the risk of missed diagnoses. Additionally, understanding air quality and its impact on overall health emphasizes the importance of reliable diagnostic tools like cortical evoked potentials. Ultimately, objective screening with cortical evoked potentials allows for reliable, early detection of hearing issues, supporting better outcomes across diverse, difficult-to-test groups.
Tracking Auditory Development in Pediatric Patients

You can use cortical auditory evoked potentials to monitor how children develop their hearing abilities over time. This approach helps identify when they reach key auditory milestones and spot any processing delays early. With this information, you can better guide interventions to support ideal auditory development. Additionally, understanding a child’s lifestyle can provide context for their auditory experiences and environment, further informing tailored strategies.
Monitoring Early Hearing Milestones
Monitoring early hearing milestones is essential for identifying potential auditory impairments and ensuring timely intervention. By tracking how your child’s brain responds to sounds, you gain neuroplasticity insights that reveal how their auditory pathways develop. Cortical mapping through cortical auditory evoked potentials helps you visualize which regions of the brain are actively processing sounds, providing a clear picture of auditory maturation. This approach allows you to detect deviations from typical development early, so interventions can be tailored effectively. Regular assessment of auditory responses not only confirms that hearing milestones are being met but also guides you in supporting ideal language and communication skills. Early monitoring with cortical auditory evoked potentials empowers you to intervene promptly, promoting better long-term outcomes for your child’s hearing health. Additionally, understanding the role of aquatic exercise can be beneficial in promoting overall well-being and stress relief during developmental assessments.
Detecting Auditory Processing Delays
Detecting auditory processing delays requires careful assessment of how children interpret and respond to sounds beyond basic hearing sensitivity. You need to evaluate their speech discrimination abilities and how well they sustain auditory attention. Cortical auditory evoked potentials help identify delays in processing speech sounds, revealing whether a child can distinguish subtle differences in phonemes. If a child’s responses show sluggish or inconsistent patterns, it may indicate that auditory processing is lagging behind their age expectations. Monitoring these aspects allows you to track developmental progress and identify potential issues early. By focusing on speech discrimination and auditory attention, you gain insight into how effectively a child processes auditory information, guiding timely interventions to support their communication skills.
Guiding Intervention Strategies
Tracking auditory development through cortical auditory evoked potentials provides valuable insights into how children are progressing in their ability to process sounds over time. By monitoring neural plasticity and changes in auditory cognition, you can tailor intervention strategies more effectively. This approach helps identify specific neural responses that indicate improved sound discrimination and processing skills. Use cortical responses to determine whether your interventions are fostering neural reorganization. Adjust therapy based on real-time data to maximize auditory skills development. Consider these key points:
- Identifying neural markers that signal progress or stagnation
- Customizing auditory training to enhance neural plasticity
- Adjusting intervention timing to optimize auditory cognition development
This targeted use of cortical potentials ensures therapies support the child’s evolving auditory system, promoting better communication outcomes.
Supporting Differential Diagnosis of Auditory Disorders
Cortical auditory evoked potentials (CAEPs) provide valuable information that can differentiate between various auditory disorders. By analyzing cortical response variability, you gain insights into neuroplasticity, revealing how the brain adapts to different pathologies. These responses help distinguish peripheral from central issues, guiding accurate diagnosis. For example, consistent CAEP patterns suggest stable neural processing, while variability indicates neuroplastic changes or dysfunction. This clarity supports tailored interventions.
| Disorder Type | Typical CAEP Pattern | Key Insight |
|---|---|---|
| Peripheral Hearing Loss | Reduced amplitude, delayed latency | Neuroplasticity insights reveal adaptation or damage |
| Central Auditory Processing | Altered response timing | Cortical response variability indicates processing issues |
| Auditory Neuropathy | Absent or abnormal CAEPs | Differentiates from sensory loss |
Guiding Hearing Aid Fitting and Management

Building on the insights gained from cortical auditory evoked potentials (CAEPs), you can optimize hearing aid fitting and management by tailoring devices to each person’s neural response patterns. CAEPs reveal how the auditory cortex processes sound, helping you understand neural plasticity and identify changes in auditory cortical maps over time. This information allows you to adjust hearing aids to promote better auditory training and neural adaptation. Consider leveraging CAEP feedback to:
Use CAEP feedback to personalize hearing aids and enhance neural adaptation for better hearing outcomes.
- Fine-tune amplification for improved speech clarity
- Monitor neural changes during auditory rehabilitation
- Personalize device settings based on cortical responses
Assessing Central Auditory Function in Adults With Neurological Conditions

Evaluating central auditory function in adults with neurological conditions is critical for understanding how brain disorders impact auditory processing. Cortical auditory evoked potentials reveal how neural synchronization and cortical processing are affected by neurological damage. By analyzing these potentials, you can identify deficits in the brain’s ability to synchronize neural activity in response to sound stimuli, which is often disrupted in conditions like stroke, multiple sclerosis, or traumatic brain injury. Changes in cortical processing patterns help determine the severity and location of neurological impairment. This assessment offers valuable insights into how well the brain processes complex sounds, speech, and auditory cues. Ultimately, it guides diagnosis, prognosis, and individualized treatment strategies for patients with neurological conditions impacting auditory function.
Research Applications in Auditory Neuroscience

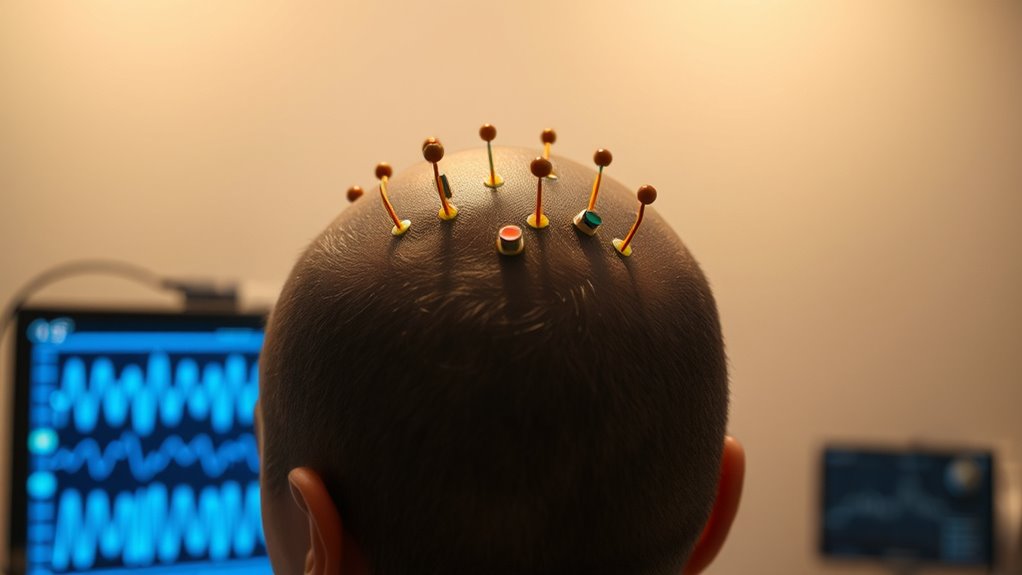
Research applications in auditory neuroscience leverage cortical auditory evoked potentials to uncover how the brain processes sound at multiple levels. You can explore neural plasticity by examining how auditory responses change with experience or training, revealing the brain’s adaptability. Cortical mapping with these potentials helps identify specific regions involved in sound perception and language processing. This approach enhances understanding of developmental and recovery processes. Key insights include:
- Tracking neural plasticity during auditory learning
- Mapping cortical responses to complex sounds
- Investigating reorganization after injury or therapy
Frequently Asked Questions
How Do Cortical Auditory Evoked Potentials Differentiate Between Types of Auditory Neuropathies?
You can differentiate between types of auditory neuropathies by examining the neural pathway responses and response latency. Cortical auditory evoked potentials reveal how well signals travel along the neural pathway, with delayed response latency indicating a disrupted or damaged pathway. By analyzing these responses, you identify whether the issue lies in synaptic transmission, neural conduction, or peripheral structures, helping tailor appropriate diagnosis and treatment strategies.
What Are the Limitations of Cortical Potentials in Diagnosing Specific Central Auditory Processing Issues?
Think of diagnosing central auditory processing issues with cortical potentials like steering through a foggy maze. You face subjectivity challenges because results can vary between patients, and equipment limitations may obscure clear readings. These factors make it hard to pinpoint specific deficits accurately. While useful, cortical potentials alone can’t always distinguish nuanced processing problems, so you should combine them with behavioral tests for a clearer picture of auditory processing health.
Can Cortical Auditory Evoked Potentials Predict Long-Term Auditory Rehabilitation Outcomes?
You might wonder if cortical auditory evoked potentials can predict long-term auditory rehabilitation outcomes. While they help with neuroplasticity assessment, their predictive power for auditory training outcomes remains limited. These potentials provide insight into brain responses but don’t reliably forecast how well someone will improve with training. Use them alongside behavioral tests to better gauge potential progress, rather than relying solely on cortical responses for long-term predictions.
How Do Cortical Responses Vary Across Different Neurological Disorders Affecting Hearing?
When exploring how cortical responses differ across neurological disorders affecting hearing, you find that each condition tells its own story. Disorders like stroke or multiple sclerosis can cause notable changes in neural plasticity and cortical reorganization. These shifts alter how your brain processes sound, making responses either exaggerated or diminished, depending on the disorder. Understanding these variations helps tailor interventions and reveals the brain’s incredible ability to adapt—sometimes better to change than you might think.
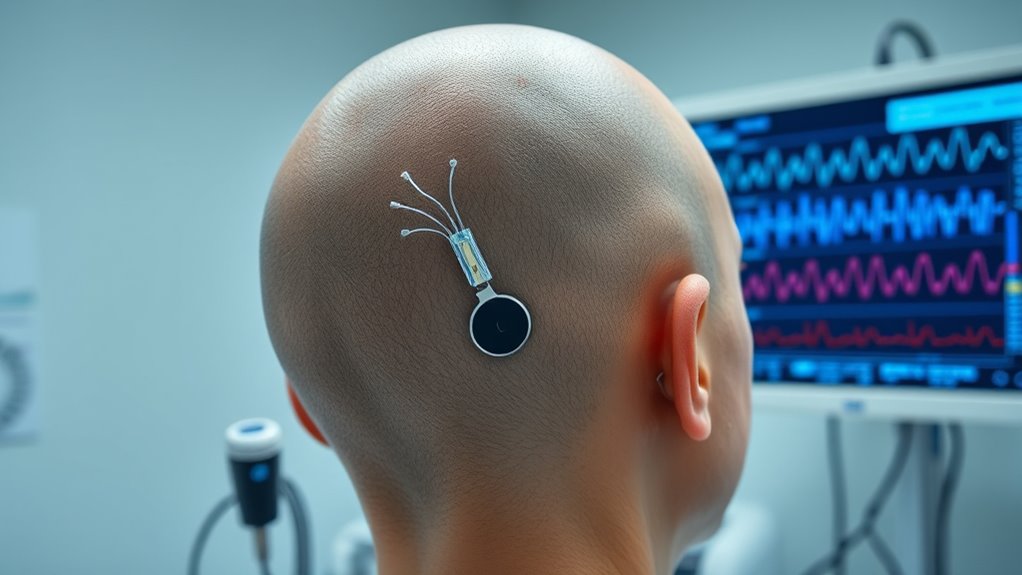
What Advancements Are Emerging in Cortical Potential Technology for Real-Time Auditory Assessment?
You’re exploring emerging advancements in cortical potential technology for real-time auditory assessment. New developments integrate brain-computer interfaces, allowing direct neural communication, and improve diagnostic imaging for more precise, immediate results. These innovations enable quicker detection of auditory issues, enhance monitoring during interventions, and facilitate personalized treatments. As technology progresses, expect more seamless, accurate assessments that transform how you diagnose and manage hearing and neurological conditions.
Conclusion
By harnessing cortical auditory evoked potentials, you open a window into the brain’s symphony of sound, revealing insights that guide diagnosis and treatment. Like a lighthouse guiding ships through foggy waters, these potentials illuminate hearing and neurological health, even in the most challenging cases. Embracing this tool empowers you to navigate complex auditory landscapes with confidence, ensuring better outcomes for patients across all ages and conditions.











