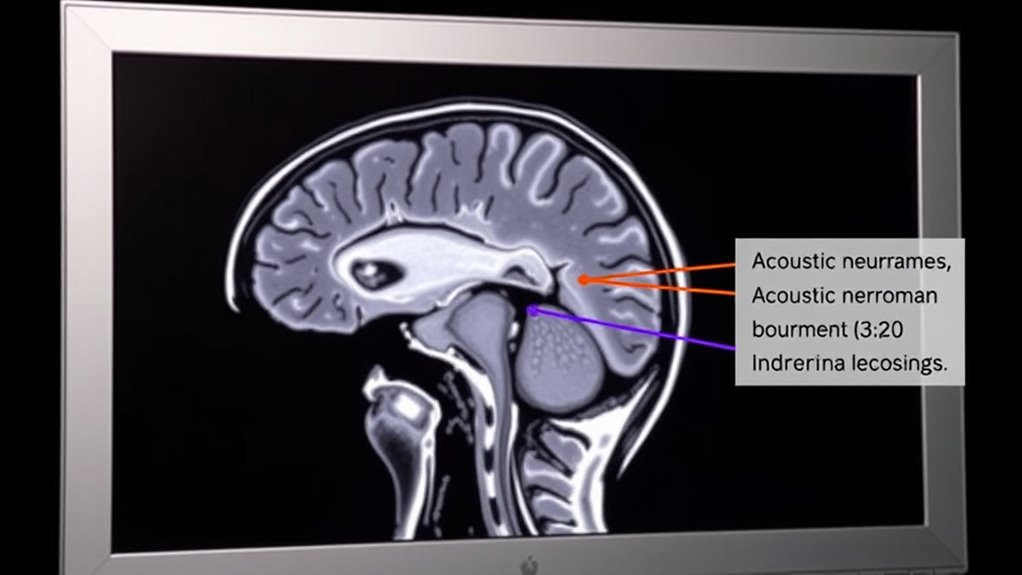
MRI helps differentiate acoustic neuromas from other tumors by revealing their typical location at the cerebellopontine angle, often involving the internal auditory canal. It shows characteristic shapes like the “ice-cream cone,” with homogeneous enhancement and specific signal patterns on T1 and T2 images. Advanced techniques, such as diffusion imaging, provide additional tissue details, making diagnosis more accurate. Exploring these features further can give you a clearer understanding of how MRI distinguishes these tumors effectively.
Key Takeaways
- MRI shows the characteristic “ice-cream cone” shape and extension into the internal auditory canal unique to acoustic neuromas.
- Homogeneous, slow, and progressive enhancement patterns on contrast MRI distinguish neuromas from other tumors with rapid enhancement.
- Signal intensity variations, such as iso- to hypointense T1 and hyperintense T2 signals, help identify acoustic neuromas.
- Advanced techniques like diffusion imaging reveal restricted water movement typical of acoustic neuromas, aiding differentiation.
- MRI’s visualization of tumor location, growth pattern, and effects on surrounding structures helps differentiate neuromas from other cerebellopontine angle masses.
The Role of MRI in Brain Tumor Detection
Magnetic Resonance Imaging (MRI) plays an essential role in detecting brain tumors, including acoustic neuromas. It provides detailed images that help identify tumor size, location, and characteristics critical for diagnosis. MRI scans can reveal specific features linked to genetic markers associated with tumor growth, aiding in understanding tumor behavior. This information is fundamental for surgical planning, allowing you and your healthcare team to determine the most effective approach. High-resolution MRI distinguishes acoustic neuromas from other intracranial abnormalities, guiding treatment decisions. By pinpointing the tumor accurately, MRI minimizes invasive procedures and improves outcomes. Additionally, penetration testing can be used to assess the security of medical imaging systems to ensure patient data protection. Overall, MRI serves as a cornerstone in early detection and precise surgical planning, making it indispensable in managing acoustic neuromas effectively.
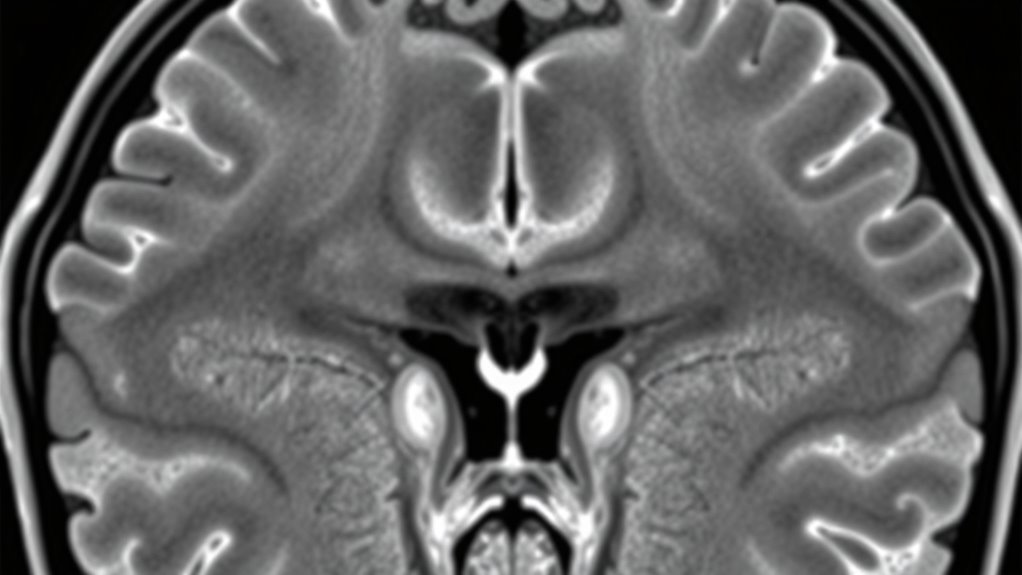
Distinguishing Acoustic Neuromas From Other Intracranial Masses
Accurate differentiation of acoustic neuromas from other intracranial masses is essential for selecting the appropriate treatment. Symptom overlap often complicates diagnosis, as many tumors share signs like hearing loss, dizziness, and balance issues. MRI helps distinguish these conditions by revealing specific features. For example:
| Acoustic Neuroma | Other Intracranial Masses |
|---|---|
| Originates at the cerebellopontine angle | May originate elsewhere in the brain |
| Typically shows internal auditory canal extension | Usually confined to a different brain region |
| Characterized by specific MRI signal patterns | Varies depending on tumor type |
Understanding these differences guides treatment options, such as surgery or radiation, tailored to each tumor’s unique features.
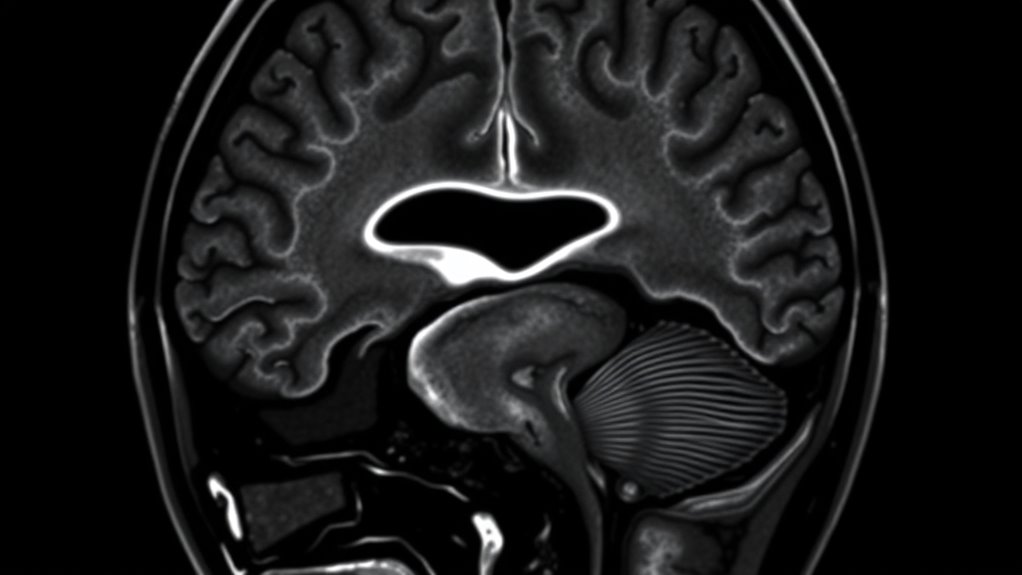
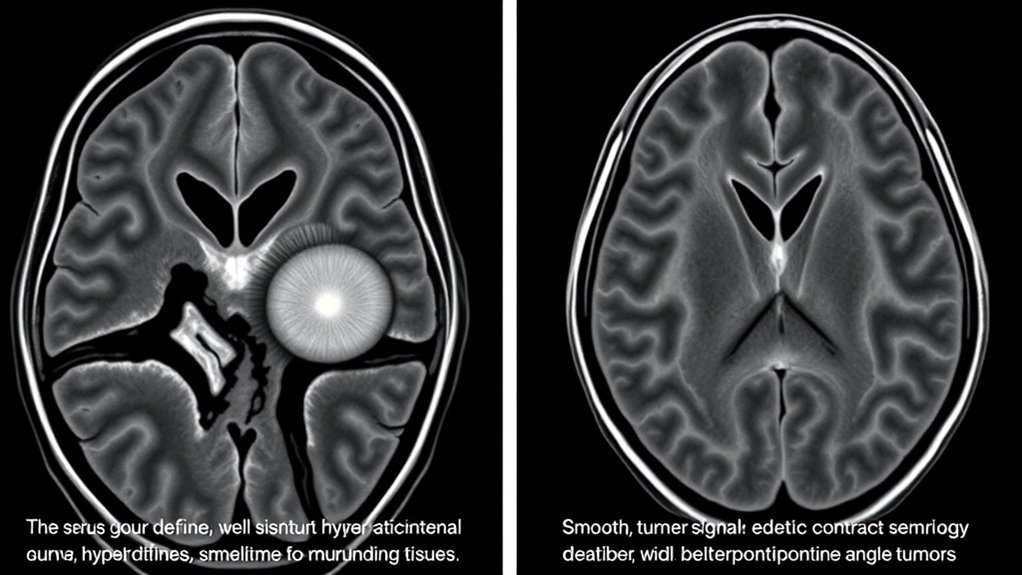
Key MRI Features of Acoustic Neuromas
Key MRI features of acoustic neuromas provide critical clues for accurate diagnosis. Typically, a vestibular schwannoma appears as a well-defined, extra-axial mass located at the cerebellopontine angle, often involving the internal auditory canal. You’ll notice it usually enlarges the canal and extends into the internal auditory meatus, indicating its origin from the vestibular portion of the cranial nerve. The tumor often shows homogeneous enhancement after contrast administration, helping differentiate it from other tumors. Its relationship with the adjacent cranial nerve is key—often displacing or compressing the nerve without invasion. Common features include a “ice-cream cone” shape and a tendency to extend into the internal auditory canal. Recognizing these MRI features is essential for distinguishing vestibular schwannoma from other intracranial masses. Additionally, understanding the typical tumor growth pattern can aid in accurate identification and treatment planning.
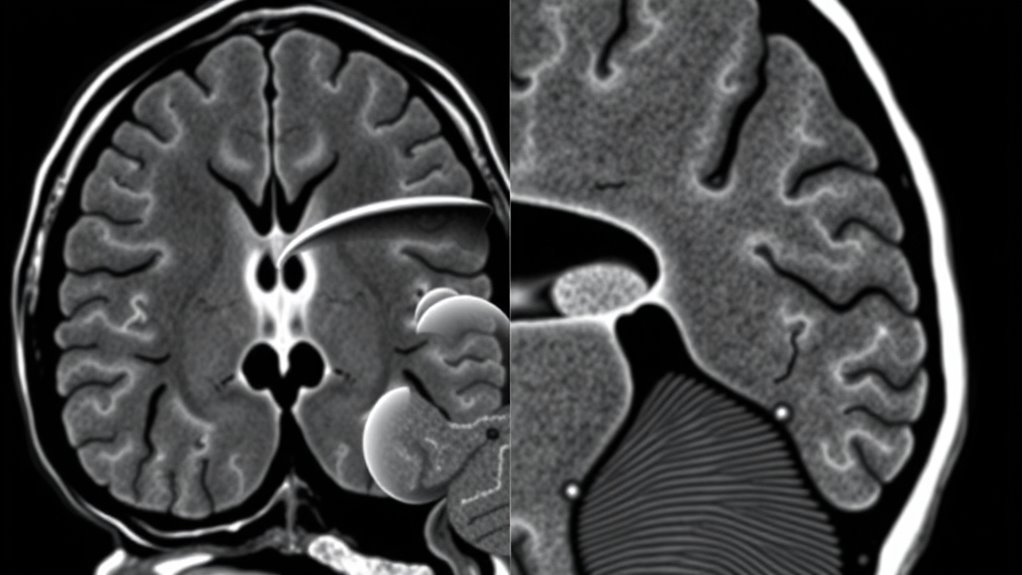
Comparing MRI Signal Characteristics of Different Tumors
When comparing tumors on MRI, you’ll notice variations in their signal intensities on different sequences. These differences help distinguish tumor types based on their tissue composition and vascularity. Recognizing distinct enhancement patterns further aids in accurate diagnosis and management. Additionally, understanding how imaging technology influences image quality and interpretation can improve diagnostic precision.
Signal Intensity Variations
Signal intensity variations on MRI play a crucial role in differentiating acoustic neuromas from other tumors. You’ll notice that acoustic neuromas generally display homogeneous signal intensity, making them stand out from more heterogeneous tumors. Tumor heterogeneity can indicate different tissue components, such as cystic areas or calcifications, which help in diagnosis. Variations in signal intensity across T1- and T2-weighted images provide clues about tumor composition. For example, a classic acoustic neuroma appears iso- to hypointense on T1 and hyperintense on T2, with minimal heterogeneity. Conversely, tumors like meningiomas may show more heterogeneous signals due to calcifications or hemorrhage. Recognizing these differences allows you to narrow down your diagnosis efficiently. Understanding tumor contrast resolution] is essential for interpreting these variations accurately.
Enhancement Patterns Differences
How do enhancement patterns on MRI help distinguish acoustic neuromas from other tumors? When you evaluate contrast enhancement, you’ll notice that acoustic neuromas typically show homogeneous or slightly heterogeneous enhancement with a slow, progressive pattern. In contrast, other tumors like meningiomas or metastases often display more intense, rapid contrast uptake, reflecting their distinct vascular patterns. Acoustic neuromas usually have less prominent vascularity, resulting in a less vigorous enhancement. Recognizing these differences allows you to differentiate tumors based on their contrast enhancement characteristics. The vascular patterns within the lesion reveal essential information: a uniform, gradual enhancement suggests an acoustic neuroma, while irregular or rapid enhancement points to alternative tumor types. This assessment is indispensable for accurate diagnosis and treatment planning.
The Importance of Tumor Location and Growth Pattern
Your understanding of an acoustic neuroma’s location and growth pattern is vital for accurate diagnosis and treatment. The tumor’s position in the brain and growth direction can affect nearby nerves and structures. Recognizing these patterns helps predict symptoms and guides surgical or radiation planning. Being aware of tumor location and growth behavior is essential for differentiating acoustic neuroma from other tumors.
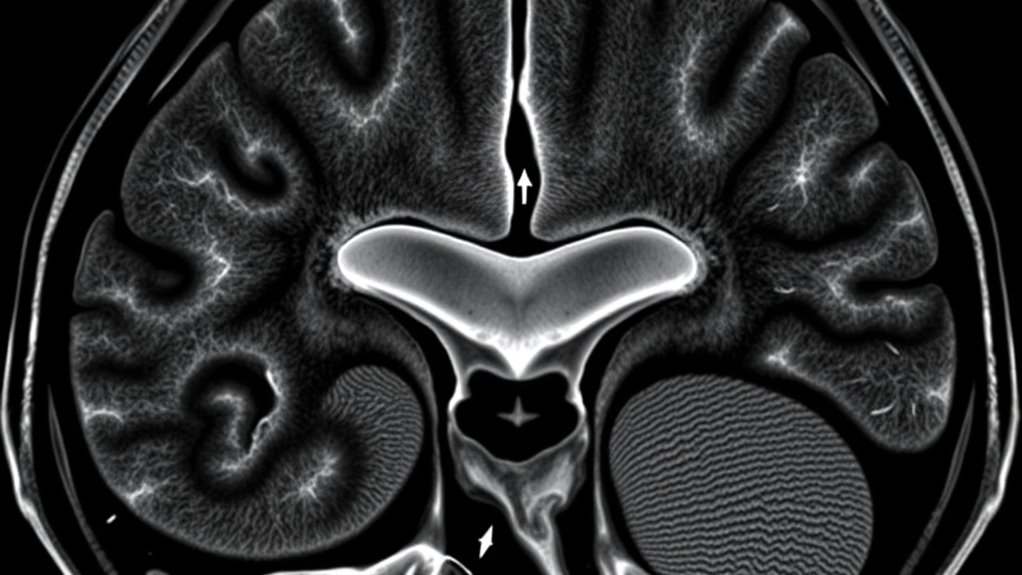
Tumor Position in Brain
The precise location and growth pattern of an acoustic neuroma considerably influence treatment options and potential outcomes. Knowing whether the tumor is near the brain stem or within the cerebellopontine angle helps determine surgical approach and prognosis. If the tumor extends into the brain stem, it may cause more neurological issues, requiring careful planning. Conversely, a tumor confined to the cerebellopontine angle might be more accessible for removal. MRI imaging clearly reveals these positions, aiding in diagnosis. Vetted imaging techniques ensure accurate assessment of tumor position and growth dynamics.
- Tumor proximity to the brain stem affects surgical risks
- Location within the cerebellopontine angle influences symptom development
- Growth pattern determines whether the tumor compresses essential structures
- Accurate positioning guides the choice between surgical removal or conservative management
Growth Direction Patterns
Why does understanding the growth direction of an acoustic neuroma matter so much? Because tumor expansion shapes symptoms and influences treatment. Recognizing whether the tumor grows toward the cerebellum or the internal auditory canal can reveal its behavior. MRI helps you visualize these patterns, guiding diagnosis and management. Consider this table:
| Growth Direction | Impact on Symptoms |
|---|---|
| Toward Brainstem | Risk of neurological deficits |
| Into Internal Auditory Canal | Hearing loss or balance issues |
| Superior/Inferior | Possible facial nerve involvement |
| Lateral/Medial | Changes in tumor size and pressure |
Knowing the tumor’s growth pattern isn’t just academic; it’s essential for predicting progression and planning effective care. Your understanding of tumor expansion directs everything from diagnosis to intervention.
Impact on Surrounding Structures
Understanding how an acoustic neuroma grows is essential because its location and direction directly affect surrounding structures like the brainstem, cerebellum, and cranial nerves. MRI reveals how the tumor’s growth pattern impacts these areas, especially concerning adjacent nerve involvement and bone erosion. If the tumor extends toward the cerebellopontine angle, it may involve nearby cranial nerves, causing facial weakness or hearing loss. In some cases, aggressive growth can lead to bone erosion of the internal auditory canal, risking further complications. Recognizing these patterns helps determine the tumor’s potential impact. Vetted conversion kits, such as the waterproof ebike system, highlight the importance of understanding growth and impact patterns when considering mechanical adaptations, emphasizing the role of detailed imaging in planning effective interventions.
- Adjacent nerve involvement can cause neurological deficits
- Bone erosion signals aggressive tumor growth
- Tumor proximity to the brainstem may affect critical functions
- Growth direction influences treatment options
Advanced MRI Techniques in Tumor Differentiation

Advanced MRI techniques have considerably improved your ability to differentiate between acoustic neuromas and other cerebellopontine angle tumors. Using contrast agents enhances tumor visibility, helping you distinguish neuromas from vascular or meningeal lesions. Diffusion imaging adds another layer of precision by measuring how water molecules move within tissues, revealing differences in tumor cellularity and structure. Acoustic neuromas typically show a characteristic pattern of restricted diffusion, setting them apart from other tumor types. These advanced techniques allow you to analyze specific tissue properties more accurately, making your diagnosis more reliable. Additionally, understanding home improvement principles such as organization and decluttering can improve the efficiency of your imaging workspace and workflow, ultimately supporting more accurate diagnostic assessments. By combining contrast-enhanced MRI with diffusion imaging, you gain critical insights into tumor composition, aiding in accurate differentiation and guiding appropriate treatment strategies.
Interpreting MRI Results for Accurate Diagnosis
Interpreting MRI results accurately is key to making a definitive diagnosis of acoustic neuroma. You need to look beyond just the tumor size and location, considering genetic markers and symptom correlation. Recognize that specific MRI features, like contrast enhancement patterns, help distinguish acoustic neuromas from other tumors. Paying attention to subtle differences can lead to better accuracy. Incorporating chemistry insights can enhance the understanding of tumor composition and behavior.
- Evaluate the tumor’s shape, margins, and signal intensity for characteristic features.
- Cross-reference MRI findings with patient symptoms, such as hearing loss or balance issues.
- Consider genetic markers linked to tumor growth and behavior for thorough assessment.
- Use advanced MRI techniques to confirm the diagnosis if initial results are inconclusive.
This thorough approach ensures you interpret results confidently, leading to precise treatment plans.
Frequently Asked Questions
Can MRI Differentiate Between Benign and Malignant Tumors?
MRI can often help you determine tumor malignancy because it provides detailed images that reveal characteristics like size, shape, and tissue composition. Its high MRI specificity allows you to distinguish benign from malignant tumors more accurately. By analyzing contrast enhancement and diffusion patterns, you can identify features suggestive of malignancy, aiding in diagnosis and treatment planning. However, sometimes additional tests are necessary for a definitive diagnosis.
How Early Can MRI Detect Small Acoustic Neuromas?
Think of MRI as a keen detective, spotting small clues early on. It can detect tiny acoustic neuromas when they’re just a few millimeters in size, making early detection possible. This means you might catch the tumor before it grows too large, aiding prompt treatment. The high-resolution imaging allows MRI to identify small tumor sizes, acting as an early warning system to protect your hearing and balance health.
Are There Specific MRI Protocols for Suspected Acoustic Neuromas?
When suspected of an acoustic neuroma, you should ask for specific MRI protocols that include high-resolution imaging and contrast enhancement. These protocols help your radiologist get detailed images of the inner ear and cerebellopontine angle, making it easier to detect small tumors. Using contrast agents improves tumor visibility, ensuring accurate diagnosis and differentiation from other types of tumors. Always specify these protocols to optimize your MRI results.
What Are Common MRI Pitfalls Leading to Misdiagnosis?
Think of MRI interpretation as steering through a maze—artifacts and interpretation errors can lead you astray. Common pitfalls include mistaking artifacts for pathology or overlooking subtle tumor features. These challenges can obscure the true picture, causing misdiagnosis. You must stay vigilant, carefully analyze images, and recognize artifact challenges to avoid false positives or negatives, ensuring accurate diagnosis of acoustic neuroma versus other tumors.
How Does MRI Compare to Other Imaging Methods Like CT or PET?
When comparing MRI to CT or PET scans, you’ll find MRI offers superior imaging resolution and contrast differentiation. MRI captures detailed soft tissue images, making it easier for you to identify acoustic neuromas and distinguish them from other tumors. CT scans, while faster and useful for bone detail, lack the soft tissue contrast MRI provides. PET scans show metabolic activity but don’t match MRI’s clarity for tumor localization and characterization.
Conclusion
Remember, MRI is your best tool for distinguishing acoustic neuromas from other tumors. By paying close attention to key features like location, signal patterns, and growth behavior, you can make accurate diagnoses. Advanced techniques further enhance your confidence. As the saying goes, “A picture is worth a thousand words”—and in medical imaging, it’s often worth a thousand diagnoses. Trust MRI to guide you toward the right identification and treatment plan.