Otoscopic AI assistants can improve the accuracy of ear examinations by analyzing images quickly and helping identify conditions. However, their reliability depends heavily on the quality and diversity of the training data, as well as rigorous validation processes. Limitations include potential biases, data gaps, and regulatory hurdles. These tools are meant to support, not replace, clinicians. To understand how these factors impact their effectiveness and safety, keep exploring the details behind their development and use.
Key Takeaways
- AI accuracy depends on diverse, high-quality training data and validation across various ear conditions and populations.
- Limitations include potential biases, variability in image quality, and challenges in recognizing rare or complex ear disorders.
- Regulatory requirements and safety standards necessitate rigorous testing, which can impact deployment and reliability.
- AI assistants are supplementary tools; they cannot replace clinical judgment or address all diagnostic nuances.
- Ongoing data collection, model refinement, and validation are essential to improve accuracy and overcome current limitations.

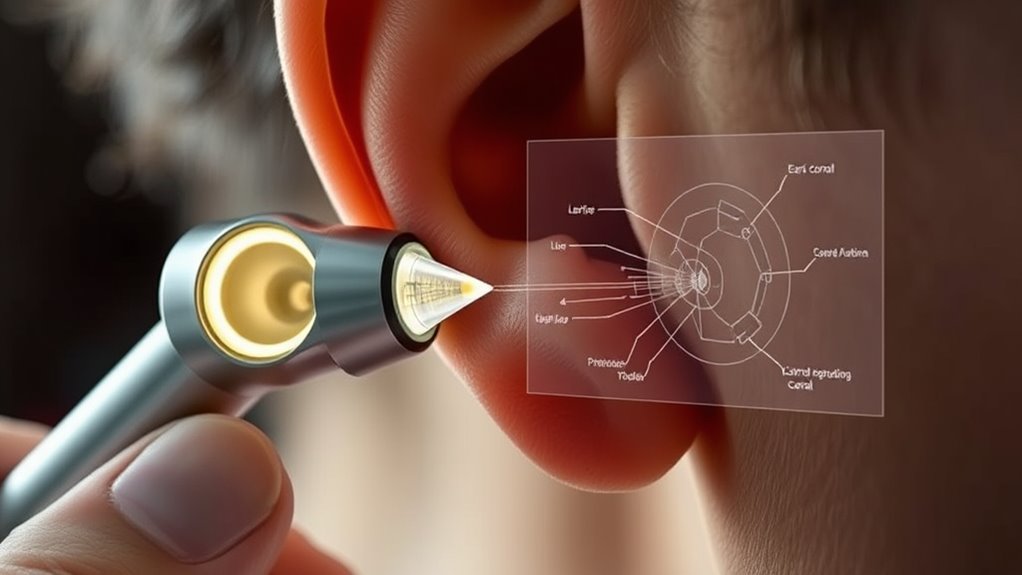
Otoscopic AI assistants are transforming how healthcare providers examine and diagnose ear conditions. These advanced tools leverage artificial intelligence to analyze images captured during ear examinations, offering the potential for quicker, more accurate assessments. However, integrating this technology into clinical practice isn’t without its challenges. One significant hurdle is training. Developing AI models that consistently produce reliable results requires vast amounts of high-quality data, which can be difficult to gather due to privacy concerns and variability in image quality. Healthcare providers and developers must invest considerable effort into training these systems to recognize a wide range of ear conditions accurately. Ensuring that the AI can handle diverse patient populations and anatomical differences is pivotal, but it’s a complex task that demands ongoing refinement and validation. Additionally, incorporating diverse training data enhances the accuracy of AI systems across different demographic groups, which is essential for equitable healthcare.
Regulatory considerations also play an essential role in the adoption of otoscopic AI assistants. As with any medical device, these tools must meet strict standards to guarantee patient safety and efficacy. Regulatory bodies, such as the FDA, require rigorous testing and validation before approval, which can slow down the deployment of innovative AI solutions. Steering through these regulatory pathways involves demonstrating that the AI performs reliably across different scenarios and that it doesn’t introduce new risks. Additionally, there’s an ongoing debate about liability—who’s responsible if an AI-assisted diagnosis misses a condition or leads to an incorrect treatment? These considerations compel developers to adhere to strict guidelines and to continuously update their systems in line with evolving regulations.
Despite these challenges, many healthcare providers see the potential benefits of otoscopic AI assistants. They can help standardize diagnoses, reduce human error, and enable quicker decision-making, especially in primary care settings where specialist access may be limited. Still, it’s essential to recognize that AI is not infallible. Limitations in training data, algorithm biases, and regulatory constraints mean that these tools are best used as supplementary aids rather than standalone solutions. As technology advances, ongoing efforts to address training challenges and regulatory considerations will be indispensable to ensuring that AI tools are both safe and effective. For now, the integration of otoscopic AI assistants into clinical workflows requires careful planning, rigorous validation, and a clear understanding of their limitations.
Frequently Asked Questions
How Do AI Assistants Compare to Expert Clinicians in Diagnosis Accuracy?
When comparing AI assistants to expert clinicians, you’ll find that AI can offer impressive diagnostic accuracy, especially in consistent pattern recognition. However, clinicians bring nuanced judgment and experience that AI may lack. While AI can support diagnosis, it’s essential to take into account the clinician comparison, as AI isn’t yet a substitute for expert judgment. Ultimately, combining AI tools with clinician expertise enhances overall diagnostic accuracy and patient care.
What Are the Common Technical Limitations of Otoscopic AI Systems?
Imagine a telescope with cloudy lenses—that’s what many otoscopic AI systems face. Their common limitations include sensor calibration issues, which affect data accuracy, and poor image quality, making diagnosis tricky. These technical hurdles hinder the AI’s ability to analyze ear images precisely. To improve, you need consistent calibration and high-quality images, ensuring the AI can better assist clinicians and deliver reliable assessments.
Can AI Assist in Diagnosing Rare Ear Conditions Effectively?
AI can assist in diagnosing rare ear conditions by enhancing rare case detection, but it faces significant AI diagnostic challenges. While AI tools improve identification of common issues, rare cases often lack enough data, making accurate diagnosis difficult. You might find AI helpful, but it shouldn’t replace expert clinical judgment. Use AI as a supplementary tool to support your decision-making, especially when rare or atypical symptoms are involved.
How Is Patient Privacy Maintained With Ai-Powered Otoscopy?
When it comes to patient privacy with AI-powered otoscopy, you’re protected through strict consent protocols that make certain patients agree to data use. Data encryption keeps images and information secure during transmission and storage, preventing unauthorized access. By following these protocols, you maintain confidentiality and trust, ensuring that sensitive ear images and data are handled responsibly while benefiting from AI assistance in diagnosis.
What Are the Costs Associated With Implementing Otoscopic AI Technology?
Think of implementing otoscopic AI technology as planting a garden—you’ll face upfront costs and careful planning. You’ll need to conduct a cost analysis to understand equipment, training, and maintenance expenses. Implementation challenges like integrating AI into existing systems and staff adaptation can be hurdles. While initial investment might seem steep, the long-term benefits, such as improved diagnostics and efficiency, make it a worthwhile endeavor.
Conclusion
As you explore otoscopic AI assistants, it’s remarkable how accuracy continues to improve, yet limitations remind us to stay cautious. Sometimes, a simple glance reveals what algorithms might miss, echoing the importance of human judgment. You might find it coincidental that in moments of technological progress, we still lean on our own intuition. Embrace these tools, but trust yourself—they’re here to assist, not replace, your keen eye and experience.