Tympanometry works by measuring how your middle ear responds to changes in air pressure, revealing how well your eardrum moves. By using a device called a tympanometer, it introduces varying pressure levels in your ear canal and tracks eardrum movement to identify any issues. This test can detect fluid buildup, infections, or pressure imbalances that affect your hearing. If you want to understand more about what tympanometry uncovers, keep exploring the details.
Key Takeaways
- Tympanometry measures how the eardrum responds to changes in air pressure, reflecting middle ear health.
- It uses a tympanometer to introduce varying pressure levels and assess eardrum movement.
- The device produces a tympanogram, a graph that reveals patterns of eardrum mobility.
- Normal tympanograms indicate proper ear function, while abnormal patterns suggest issues like fluid or perforation.
- By analyzing tympanograms, clinicians can diagnose middle ear problems, pressure imbalances, and infections.

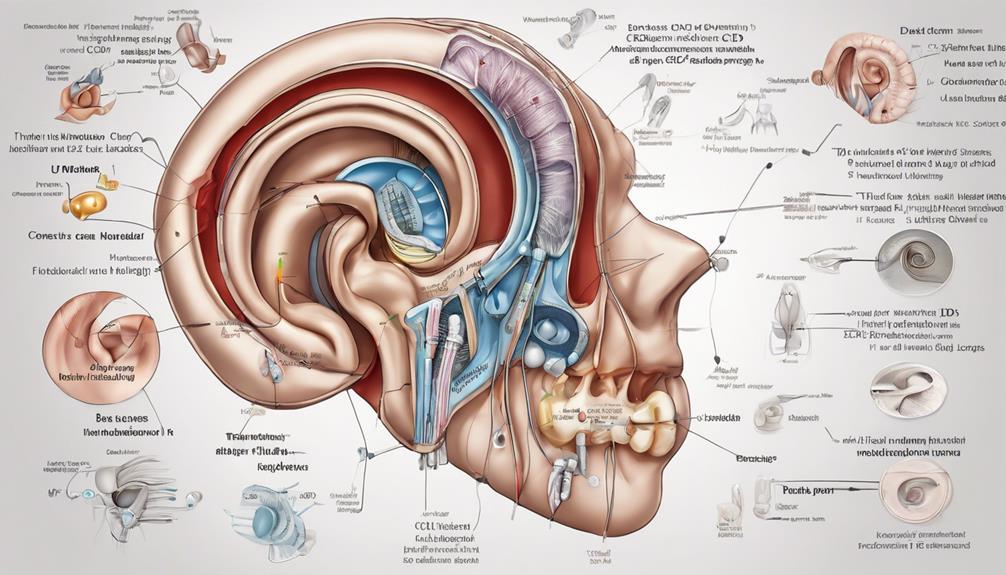
Tympanometry is a quick and non-invasive test that reveals important information about your middle ear’s health. When you undergo this test, you’re essentially measuring how well your middle ear functions, especially how it handles ear pressure. The middle ear is a small, air-filled space behind your eardrum that plays a vital role in hearing and balance. By assessing how your eardrum responds to changes in air pressure, tympanometry provides insights into whether your middle ear is operating properly.
During the test, a device called a tympanometer is placed in your ear canal. It gently introduces varying levels of air pressure while a probe measures the movement of your eardrum. This movement is directly related to the pressure inside your middle ear. If your middle ear has normal ear pressure, your eardrum will move freely in response to the pressure changes, producing a characteristic pattern on the tympanogram. Conversely, if there’s an imbalance—such as fluid buildup, infection, or a perforation—the eardrum’s movement will be restricted or abnormal, signaling a problem.
A tympanometer measures eardrum movement in response to air pressure changes, indicating middle ear health.
One of the main things this test reveals is whether your middle ear has the correct amount of ear pressure. Proper ear pressure is essential for ideal hearing and preventing discomfort. When the pressure is too high or too low, it can cause sensations of fullness, muffled hearing, or even pain. Tympanometry helps identify these issues quickly, which can be vital for diagnosing conditions like middle ear infections, eustachian tube dysfunction, or fluid accumulation.
The test also helps determine if there’s fluid in the middle ear, a common cause of hearing loss in children and adults alike. Fluid acts as a barrier, preventing the eardrum from moving normally, which this test can detect. Additionally, tympanometry can identify if the eardrum is perforated or if there’s scarring that might impede its movement.
Frequently Asked Questions
How Accurate Is Tympanometry in Detecting Early Middle Ear Issues?
Tympanometry offers good clinical accuracy for detecting early middle ear issues, making it a valuable tool for early detection. It measures how well your eardrum moves in response to pressure changes, identifying problems like fluid buildup or eustachian tube dysfunction before symptoms appear. While not perfect, it’s a reliable method to catch issues early, helping you seek timely treatment and prevent more serious complications.
Can Tympanometry Differentiate Between Types of Ear Infections?
They say, “A picture is worth a thousand words,” and tympanometry helps you see ear issues clearly. While it can identify the presence of an ear infection, it doesn’t differentiate between ear infection types. Its diagnostic accuracy is high for detecting middle ear problems overall, but for specific infection types, your doctor may need additional tests. Tympanometry is a helpful tool, but not a standalone solution for detailed diagnosis.
What Are the Limitations of Tympanometry in Diagnosing Hearing Problems?
You should know that tympanometry has limitations when diagnosing hearing problems. Subjectivity limitations can affect results, as interpretations may vary between clinicians. Equipment variability also plays a role, with different devices sometimes providing inconsistent data. These factors mean you shouldn’t rely solely on tympanometry for diagnosis. Instead, combine it with other tests and clinical evaluations to get a more accurate understanding of your hearing health.
How Does Age Affect Tympanometry Results?
Imagine your ears as a finely tuned instrument whose strings loosen with age. Age-related changes can subtly alter your middle ear’s responsiveness, making tympanometry accuracy less precise. As you grow older, the eardrum and ossicles may stiffen, affecting results. Consequently, age influences tympanometry, requiring clinicians to interpret findings within the context of natural aging to avoid misdiagnosis.
Is Tympanometry Safe for All Age Groups, Including Infants?
Tympanometry is generally safe for all age groups, including infants, but pediatric considerations are essential. You should guarantee safety protocols are followed, especially with infants, to prevent discomfort or distress. Professionals are trained to use gentle techniques and appropriate equipment. If used correctly, tympanometry provides valuable insights without risk, making it a safe, non-invasive test for diagnosing middle ear issues across all ages, including the youngest patients.
Conclusion
Tympanometry may seem simple, but it uncovers complex details about your hearing health. Like a window into your middle ear, it reveals issues hidden beneath the surface. While the test is quick and painless, its insights can be profound—highlighting problems you might not notice otherwise. Remember, what it shows isn’t just data; it’s your body’s way of telling you to listen closer, to care more. Sometimes, the smallest test reveals the biggest truths.