Multidisciplinary clinics streamline complex hearing diagnoses by bringing together specialists like audiologists, ENT doctors, and speech therapists to work collaboratively. This team approach guarantees quick, accurate assessments and personalized treatment plans, while improving communication and patient engagement. Advanced diagnostic tools such as MRI scans and data sharing also enhance precision. If you’re interested, you’ll discover how future trends and innovative strategies are shaping even more effective hearing healthcare solutions.
Key Takeaways
- Multidisciplinary clinics facilitate coordinated collaboration among audiologists, ENT specialists, and speech therapists for comprehensive hearing assessments.
- Advanced diagnostic tools like high-resolution MRI and integrated data systems enable precise, holistic evaluation of complex hearing conditions.
- Effective communication, shared digital platforms, and optimized scheduling streamline workflows and reduce diagnostic delays.
- Incorporating telehealth and AI technologies enhances diagnostic accuracy, accelerates treatment planning, and improves patient access.
- Interdisciplinary teamwork and patient engagement lead to personalized treatment strategies and higher satisfaction in complex hearing cases.
The Role of Multidisciplinary Teams in Hearing Healthcare

Multidisciplinary teams play a crucial role in hearing healthcare by bringing together professionals from various fields to deliver thorough patient care. Your team members, including audiologists, ENT specialists, and speech therapists, must prioritize interdisciplinary communication to guarantee everyone is on the same page. Clear communication helps coordinate diagnoses, treatment plans, and follow-up steps efficiently. As a patient, you benefit from this collaboration through extensive patient education, where each specialist explains different aspects of your condition and solutions, empowering you to make informed decisions. This teamwork ensures no detail slips through the cracks, streamlining your experience and optimizing outcomes. Ultimately, effective collaboration and patient education within multidisciplinary teams create a seamless, personalized approach to hearing healthcare. Additionally, understanding the waves and wind involved in auditory processes can enhance the team’s ability to address complex hearing issues comprehensively.
Benefits of Collaborative Approaches for Complex Cases

When managing complex hearing health cases, collaboration among specialists leads to more accurate diagnoses and effective treatment strategies. Working together enhances patient engagement, making individuals feel involved and informed throughout their care. Additionally, integrated teams leverage technology to share data seamlessly, improving decision-making. The benefits include: 1. Improved Diagnostic Accuracy: Combining expertise reduces misdiagnoses and uncovers underlying issues. 2. Personalized Treatment Plans: Collaborative input tailors interventions to each patient’s unique needs. 3. Enhanced Patient Experience: Active engagement and technology use foster trust, satisfaction, and adherence. Moreover, understanding advanced diagnostic tools such as flat iron bike can aid in comprehensive assessments and treatment planning.
Diagnostic Tools and Technologies in Integrated Clinics

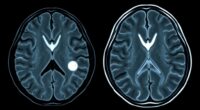
How do clinics make certain of accurate diagnoses and effective treatment plans? They leverage advanced diagnostic tools and technologies. Imaging advancements, like high-resolution MRI and CT scans, provide detailed visuals of inner ear structures, helping pinpoint issues with precision. These imaging techniques allow specialists to visualize anomalies that might be missed with traditional exams. Additionally, data integration plays an indispensable role, combining test results, patient history, and imaging data into a comprehensive view. This seamless integration enables clinicians to identify patterns quickly, reducing diagnostic errors. Modern clinics also use specialized audiometric tools and electrophysiological testing to assess hearing function thoroughly. Comprehensive assessment is essential for capturing the full scope of complex hearing issues. Together, these technologies streamline the diagnostic process, ensuring you receive targeted, effective treatment based on accurate, holistic insights into your hearing health.
Case Studies Demonstrating Improved Patient Outcomes

Real-world case studies show how integrated diagnostic approaches lead to better patient outcomes. When multiple specialists collaborate, they can identify issues earlier and develop more effective treatment plans. These successes highlight the power of teamwork in improving healthcare results. Incorporating multidisciplinary collaboration in diagnosis processes is essential for achieving accurate and timely hearing assessments.
Integrated Diagnostic Approaches
Integrated diagnostic approaches in multidisciplinary clinics have consistently led to better patient outcomes by combining expertise and advanced technologies. By engaging patients actively, you foster trust and guarantee their concerns guide the diagnostic process. Technological integration enables seamless data sharing among specialists, reducing delays and improving accuracy. For example:
- Collaborating across audiology, neurology, and radiology streamlines complex diagnoses, leading to quicker, more precise treatments.
- Incorporating advanced imaging and audiometric tools enhances detection of subtle or overlapping conditions.
- Engaging patients with clear communication and involving them in decisions boosts satisfaction and adherence.
- Recognizing relationships and emotional bonds can be crucial in understanding patient concerns and improving diagnostic accuracy.
These approaches demonstrate that multidisciplinary methods with integrated technology and patient engagement not only improve diagnoses but also enhance overall care experiences, leading to better health outcomes.
Collaborative Care Success
Have you ever wondered how multidisciplinary clinics turn complex diagnoses into successful treatments? It often comes down to collaborative care and how well patient engagement is prioritized. When teams from audiology, ENT, and psychology work together seamlessly, patient outcomes improve markedly. Funding models that support integrated services make this collaboration possible, ensuring resources are allocated efficiently. Case studies show that patients experience faster diagnoses, better treatment adherence, and higher satisfaction when they feel involved in their care. These clinics foster open communication, empowering patients to participate actively in decision-making. As a result, treatment plans become more personalized and effective. Understanding Prophetic Dreams can also inspire a new perspective on intuitive insights within healthcare. Ultimately, the success of these clinics highlights how a team approach, backed by appropriate funding, can transform complex hearing diagnoses into positive, life-changing outcomes.
Challenges and Solutions in Implementing Multidisciplinary Clinics

Implementing multidisciplinary clinics can be challenging, especially when coordinating specialist teams and managing logistical hurdles. You need to find effective ways to streamline communication and align schedules across different disciplines. Addressing these barriers is essential for providing seamless, patient-centered care. Incorporating efficient communication strategies can significantly improve team collaboration and patient outcomes.
Coordinating Specialist Teams
Coordinating specialist teams in multidisciplinary clinics often presents significant challenges, as aligning diverse expertise and workflows requires careful planning and communication. To succeed, focus on effective interdisciplinary communication, ensuring everyone shares updates and goals clearly. Additionally, developing solid funding strategies helps sustain the team’s collaborative efforts.
Consider these key approaches:
- Establish regular interdisciplinary meetings to foster open communication and coordination.
- Implement shared digital platforms for seamless information exchange among team members.
- Secure diverse funding sources, including grants and institutional support, to cover team activities and resources.
Managing Logistical Barriers
Managing logistical barriers in multidisciplinary clinics often requires addressing complex scheduling, space limitations, and resource allocation challenges that can disrupt seamless collaboration. You’ll need to optimize appointment scheduling to reduce delays and ensure patients see all specialists efficiently. Coordination is key—aligning providers’ availability minimizes gaps and overlaps. Space limitations may require creative solutions like shared rooms or flexible use of available areas to accommodate multiple specialists. Proper resource allocation ensures essential tools and personnel are available without overextending your clinic’s capacity. Regular communication among team members helps identify bottlenecks early. Additionally, implementing effective resource management strategies can enhance overall efficiency and patient care. By streamlining appointment scheduling, maximizing space, and carefully manage resources, you can overcome logistical hurdles and facilitate smoother, more effective multidisciplinary collaborations.
Future Trends in Hearing Diagnosis and Treatment Collaboration

As technology advances, collaboration between audiologists, ENT specialists, and other healthcare providers is set to become more seamless and integrated, transforming how hearing diagnosis and treatment are approached. Telehealth advancements enable remote consultations, making expert care accessible regardless of location. Personalized medicine will tailor treatments based on genetic and individual data, improving outcomes. To stay ahead, you’ll see:
- Increased use of telehealth platforms for real-time, multidisciplinary assessments.
- Integration of AI-driven diagnostics for faster, more accurate diagnoses.
- Development of personalized treatment plans that combine genetic information with traditional audiological data.
- The adoption of Vetted – Halloween Product Reviews to enhance patient engagement and education about hearing health options.
These trends will streamline workflows, reduce delays, and enhance patient-centered care, making hearing health management more efficient and effective.
Frequently Asked Questions
How Are Patient Privacy and Data Shared Securely Among Team Members?
You guarantee patient privacy and data sharing are secure by using electronic records with robust data encryption. This protects sensitive information when team members access or exchange data. You follow strict protocols and access controls, so only authorized personnel can view or modify records. Regular audits and secure login methods help maintain confidentiality, giving patients confidence that their hearing diagnoses stay private while allowing seamless collaboration among your healthcare team.
What Training Is Required for Staff Working in Multidisciplinary Hearing Clinics?
You need to complete training in interdisciplinary collaboration to work effectively in a multidisciplinary hearing clinic. Staff should also pursue specialized certification relevant to audiology, ENT, or speech therapy to guarantee expertise. This training helps you communicate clearly, share patient data securely, and coordinate care seamlessly, ultimately improving patient outcomes. Continuous education on best practices and confidentiality is essential to stay current and maintain high standards in this collaborative environment.
How Are Appointments Coordinated Across Different Specialists Efficiently?
Think of appointment scheduling as conducting an orchestra—you need harmony among all players. You coordinate appointments by using integrated scheduling systems that share real-time updates, ensuring no overlaps or gaps. Efficient interdisciplinary communication is essential; it keeps everyone informed of patient progress and upcoming needs. With clear communication channels and synchronized calendars, you create a seamless flow, allowing specialists to work together smoothly and deliver all-encompassing, timely care for complex hearing cases.
What Funding Models Support the Sustainability of Multidisciplinary Clinics?
You should consider funding models that include all-encompassing insurance coverage and innovative billing strategies. These models guarantee sustainability by covering the costs of multidisciplinary services. You can explore bundled payments or value-based care approaches that streamline billing and reduce administrative burdens. By securing diverse funding sources, including grants or subsidies, you’ll maintain the clinic’s financial health while providing integrated, patient-centered care for complex hearing diagnoses.
How Is Patient Satisfaction Measured in Complex Hearing Diagnosis Clinics?
You can measure patient satisfaction in complex hearing diagnosis clinics through patient feedback and satisfaction surveys. These tools allow you to gather direct insights on patients’ experiences, including clarity of communication, wait times, and overall care quality. By analyzing survey results regularly, you can identify areas for improvement, enhance patient-centered care, and guarantee that your clinic effectively meets patients’ needs and expectations.
Conclusion
Imagine your hearing journey as steering a complex maze. Multidisciplinary clinics act as your trusted compass, guiding you smoothly through twists and turns. With every expert working together, you find clearer paths and brighter outcomes. Embrace this collaborative voyage, where technology and teamwork light the way. Together, you’ll reach the heart of accurate diagnosis and effective treatment, transforming a confusing maze into a well-marked trail toward better hearing and quality of life.