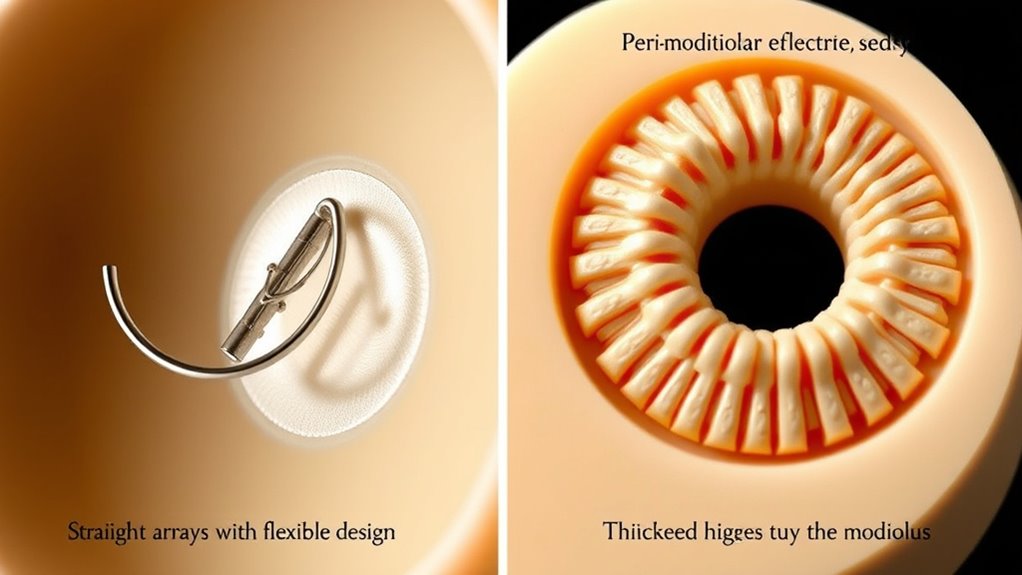
Straight electrode arrays are flexible and easier to insert, often positioned farther from the modiolus, which can affect sound clarity but reduce insertion trauma. Perimodiolar arrays are pre-curved to hug the modiolus closely, enhancing neural stimulation and speech perception but may pose higher insertion risks. Understanding these differences helps you choose the best option for your needs. Exploring further reveals how these designs impact surgical techniques and hearing outcomes.
Key Takeaways
- Straight arrays are linear, flexible, and easier to insert, often used for broader cochlear coverage and residual hearing preservation.
- Perimodiolar arrays are pre-curved, designed to hug the modiolus, positioning electrodes closer to neural tissue for precise stimulation.
- Placement differences influence sound clarity: perimodiolar arrays offer better high-frequency perception, while straight arrays provide broader coverage.
- Straight arrays typically have lower manufacturing costs and are associated with reduced insertion trauma compared to pre-curved arrays.
- Choice between designs depends on patient anatomy, hearing needs, and surgical considerations for optimal implant performance.
Overview of Cochlear Implant Electrode Arrays
Cochlear implant electrode arrays are essential components that directly influence the device’s performance and the patient’s hearing outcomes. The electrode material plays a fundamental role, affecting both durability and biocompatibility. Common materials like platinum are chosen for their excellent electrical conductivity and safe integration within the cochlea. Patient comfort is also a key factor; a well-designed electrode array minimizes trauma during insertion and reduces irritation afterward. The array’s flexibility and size can impact comfort levels, making it easier for patients to acclimate to the device. Whether straight or perimodiolar, these arrays are engineered to optimize sound transmission while ensuring minimal discomfort. The design of the electrode array can also influence the effectiveness of tuning and customization, ultimately improving hearing results and patient satisfaction.
Structural Characteristics of Straight and Perimodiolar Designs

Understanding the structural features of straight and perimodiolar electrode arrays helps you appreciate their placement within the cochlea. Each design uses distinct positioning strategies that influence how they interact with auditory nerve fibers. Examining their structural design features reveals how these differences impact performance and outcomes. Notably, electrode array positioning plays a crucial role in optimizing auditory nerve stimulation and overall device efficacy.
Electrode Positioning Strategies
The placement of electrode arrays within the cochlea markedly influences their performance, with each design offering distinct structural advantages. Straight arrays tend to be inserted more easily, reducing biocompatibility issues, but may not position as close to the modiolus. Perimodiolar arrays are designed to hug the modiolus, enhancing signal precision but increasing manufacturing costs and potential trauma. To optimize results, consider these strategies:
- Prioritize gentle insertion techniques to minimize tissue damage and biocompatibility concerns.
- Balance the benefits of close proximity to neural tissues with the risks of trauma during placement.
- Account for manufacturing costs when selecting a design that aligns with both clinical needs and budget constraints.
- Understanding Vetted – Halloween Product Reviews can provide insights into selecting the most suitable and cost-effective array designs.
These strategies ensure effective positioning, maximizing hearing outcomes while managing risks and costs.
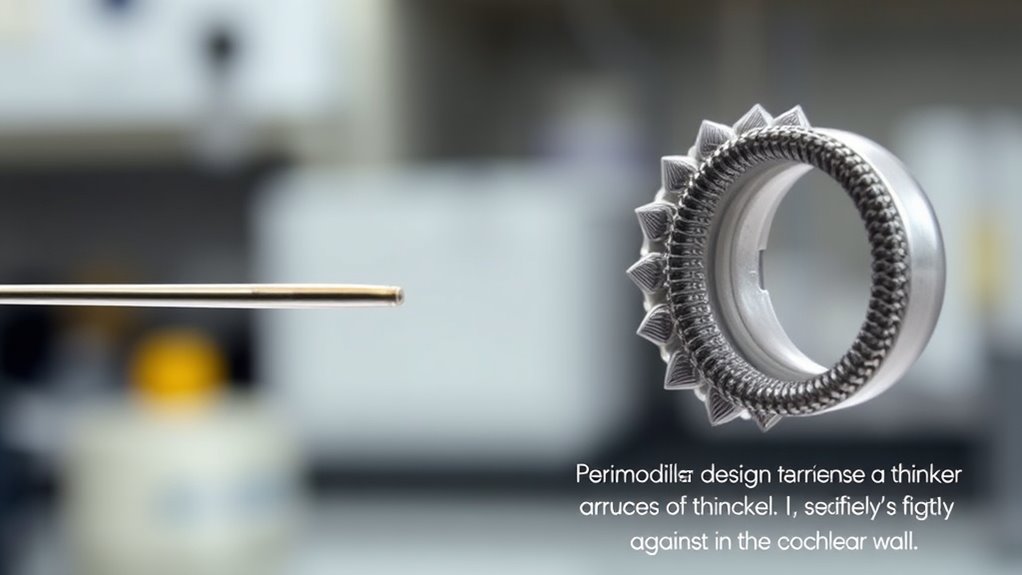
Structural Design Features
Straight electrode arrays are characterized by their linear, flexible design, which allows for easier insertion and navigation through the cochlear spiral. They typically feature a slim profile, promoting biocompatibility and reducing biocompatibility issues. In contrast, perimodiolar designs have a curved, pre-curved structure that hugs the modiolus, providing closer proximity to neural tissue. Manufacturing precision is vital for both types to guarantee proper placement and minimize trauma. The table below highlights key structural features:
| Feature | Straight Arrays | Perimodiolar Arrays | Impact |
|---|---|---|---|
| Flexibility | High, allows easy insertion | Moderate, pre-curved for close contact | Balances ease of insertion with stability |
| Shape | Linear, straight | Curved, pre-curved | Affects placement and biocompatibility issues |
| Material | Silicone, platinum contacts | Similar, with precise manufacturing | Ensures durability and safety |
| Biocompatibility | Generally good, depends on design | Similar, design affects tissue response | vital for long-term success |
| Manufacturing Precision | Essential for accurate placement | vital for pre-curved design | Reduces trauma, enhances performance |
A new sentence with material selection and the rest of the sentence.
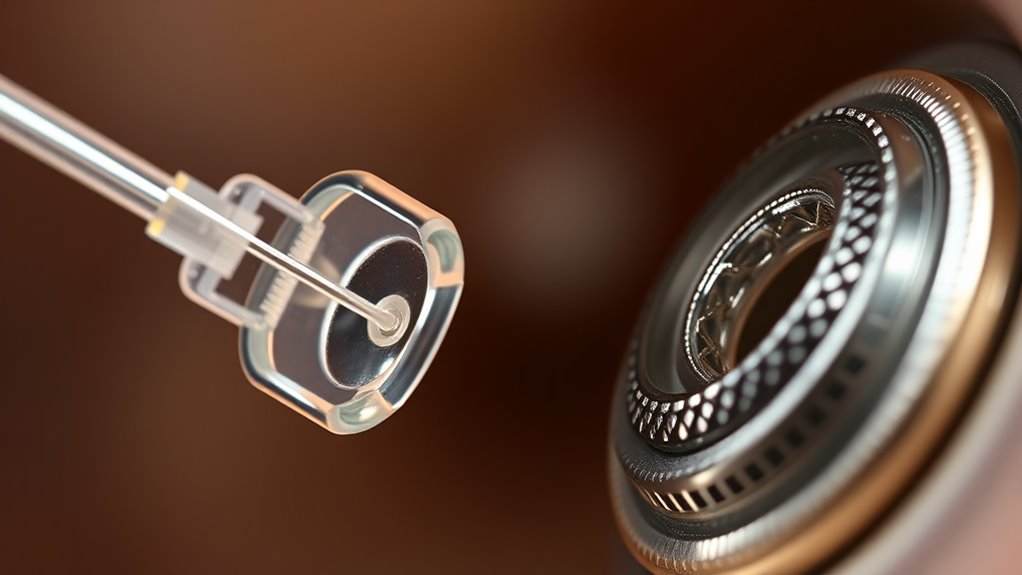
Surgical Techniques and Insertion Methods

You need to choose the appropriate surgical approach based on the electrode design and patient anatomy. Insertion techniques can vary considerably, presenting unique challenges for each type. Understanding these variations helps guarantee proper placement and minimizes complications during surgery. Additionally, selecting a suitable implant and considering the patient’s overall health can significantly influence the success of the procedure.
Surgical Approach Variations
Choosing the right surgical approach is essential in maximizing electrode array placement and patient outcomes. Surgical approach variations allow for patient-specific customization, ensuring the technique suits individual anatomy and needs. Consider these key factors: 1. Anatomical differences influence whether a cochleostomy or round window approach is best. 2. Variations in cochlear size and shape guide your choice of access route. 3. Patient history and cochlear health help determine the most suitable approach for ideal positioning. Additionally, understanding electrode array design can influence the surgical strategy by aligning the approach with the array’s characteristics for optimal placement.
Insertion Technique Challenges
Despite advances in electrode array design, insertion technique challenges remain a critical factor in cochlear implant success. You must carefully manage the insertion angle to prevent trauma and guarantee proper placement. An incorrect angle can increase the risk of scar tissue formation, which can impair electrode function and reduce hearing outcomes. Gentle, controlled insertion minimizes trauma and helps avoid damaging delicate cochlear structures. You should also be aware that excessive force or rapid insertion can lead to dislocation or fracture of the electrode array. Proper training and understanding of the insertion techniques are essential for minimizing complications and ensuring optimal device performance. Mastering precise insertion techniques reduces complications and promotes ideal positioning. Overall, attention to the insertion angle and gentle handling are essential in overcoming these challenges and ensuring long-term device performance.
Electrical Stimulation and Neural Activation

Electrical stimulation in cochlear implants directly influences neural activation by delivering targeted electrical pulses to the auditory nerve fibers. Your electrode-tissue interaction plays a vital role in shaping neural activation patterns, affecting how effectively sound is perceived. Proper contact ensures precise stimulation, reducing current spread and avoiding unintended activation. To optimize neural responses, consider these factors:
- Electrode positioning influences the specificity of neural activation.
- Tissue impedance impacts current delivery and pattern fidelity.
- Stimulus parameters shape the clarity and accuracy of perceived sounds.
- Somatic therapy techniques can help manage the stress and trauma related to hearing loss and medical procedures, supporting overall well-being.
Understanding these elements helps you refine stimulation strategies, improving the interface between electrodes and neural tissue. This, in turn, enhances the overall auditory experience by fostering more natural and focused neural activation, leading to better sound perception and clearer hearing outcomes.
Performance Outcomes and Sound Quality

The design of electrode arrays considerably impacts the performance outcomes and sound quality experienced by cochlear implant users. Straight arrays often provide broader coverage, which can enhance speech perception in complex listening environments. Perimodiolar arrays position closer to the modiolus, improving neural stimulation and resulting in clearer, more focused sound. This proximity tends to boost sound clarity, especially in noisy settings. Users with perimodiolar designs often report better speech perception, especially for high-frequency sounds. Conversely, straight arrays may be advantageous for preserving residual hearing, but they might offer slightly less precise sound quality. Additionally, understanding passive voice detection can help improve clarity and engagement in your writing. Overall, the electrode array choice influences how effectively you perceive speech and sounds, directly affecting your listening experience and communication abilities.
Risks, Complications, and Considerations
Choosing the right electrode array involves weighing potential risks and complications that can affect your safety and hearing outcomes. Infection risks are a concern, especially if proper sterile techniques aren’t followed. Electrode migration, where the array shifts from its original position, can impair hearing performance and may require revision surgery. Consider these key points:
- Infection risks can lead to complications if not promptly managed.
- Electrode migration might cause reduced sound quality or the need for additional procedures.
- Patient anatomy and surgical technique influence the likelihood of complications.
Being aware of these risks helps you make informed decisions and prepares you to discuss concerns with your surgeon. While both straight and perimodiolar arrays have unique profiles, understanding potential complications ensures safer, more effective outcomes.
Suitability for Different Patient Profiles

Selecting the appropriate electrode array depends heavily on individual patient characteristics and needs. For patient selection, consider factors like cochlear anatomy, residual hearing, and age. Straight arrays often suit patients with broader cochleae or preserved residual hearing, providing easier insertion and less trauma. Perimodiolar arrays may be better for patients needing more precise stimulation, especially if cochlear ossification limits electrode placement. Cost considerations also influence choice; perimodiolar arrays tend to be more expensive but may offer improved outcomes for certain profiles. Balancing these factors ensures you choose an array tailored to the patient’s anatomy and hearing needs. Ultimately, understanding each patient’s unique profile helps optimize hearing restoration while managing costs effectively. Additionally, awareness of AI security vulnerabilities is crucial when integrating advanced technologies into medical devices to ensure patient safety.
Advances in Electrode Array Technology

Recent innovations in electrode array technology have markedly enhanced cochlear implant performance by improving insertion precision, reducing trauma, and expanding candidacy options. These advancements include flexible materials and optimized designs that address biocompatibility issues, ensuring better tissue integration and fewer adverse reactions. Additionally, manufacturers are working to lower manufacturing costs without compromising quality, making implants more accessible. Understanding these developments helps you appreciate how they impact patient outcomes. Key points include:
- Use of biocompatible materials minimizes immune responses and enhances longevity.
- Precision engineering reduces trauma during insertion, preserving residual hearing.
- Cost-effective manufacturing techniques improve availability and affordability.
These technological strides are shaping a future where cochlear implants are safer, more reliable, and accessible to a broader range of candidates.
Future Directions in Electrode Array Development

Building on recent technological advancements, future electrode array development aims to further enhance cochlear implant outcomes through innovative designs and materials. Expect biocompatibility improvements that reduce tissue response and increase longevity. Wireless connectivity will become standard, enabling seamless data transfer and real-time adjustments. This evolution allows for more personalized auditory experiences and easier maintenance. Developers are exploring flexible, ultra-thin arrays that conform better to cochlear anatomy, minimizing trauma. Additionally, integrating sensors can provide feedback on electrode placement and function. The table below highlights key future directions:
| Focus Area | Benefits |
|---|---|
| Biocompatibility improvements | Reduced tissue response, longer device lifespan |
| Wireless connectivity | Enhanced user experience, real-time updates |
| Advanced materials | Flexibility, durability, lower trauma |
Frequently Asked Questions
How Do Electrode Array Choices Influence Long-Term Device Durability?
You might wonder how electrode array choices impact long-term device durability. The type you select influences electrode longevity by affecting how well the device withstands daily use and environmental factors. Material resilience plays a vital role, as durable materials resist wear and corrosion over time. By choosing an array with high-quality materials, you can help guarantee your cochlear implant remains effective and reliable for years to come.
What Are the Cost Differences Between Straight and Perimodiolar Arrays?
Think of cost differences as a journey through a maze; straight arrays often cost less, while perimodiolar designs can be pricier. You’ll find that electrode material and manufacturing complexity drive these costs—perimodiolar arrays typically involve more intricate manufacturing, raising expenses. While straight arrays are simpler and cheaper, perimodiolar designs may offer better placement, justifying their higher price. Your choice impacts both budget and clinical outcome.
Are Certain Electrode Designs Better Suited for Pediatric Patients?
You should consider that certain electrode designs better suit pediatric patients due to their unique anatomical considerations and childhood hearing development needs. Perimodiolar arrays often provide closer proximity to the cochlear nerve, enhancing stimulation efficiency vital for developing auditory pathways. Straight arrays may be easier to insert in smaller cochleae, reducing trauma. Tailoring your choice based on pediatric anatomy helps optimize hearing outcomes and supports ongoing childhood development.
How Do Electrode Arrays Impact MRI Compatibility?
Think of your cochlear implant like a delicate radio; MRI safety is vital to prevent electrical interference. Electrode arrays influence this—perimodiolar designs are often closer to the nerve, which can complicate MRI procedures, increasing the risk of electrical interference. Straight arrays tend to be more compatible, reducing MRI risks. Your choice affects not just hearing but also your safety during imaging, so consult your specialist about the best options for MRI compatibility.
What Considerations Determine the Optimal Electrode Array for Individual Anatomy?
When choosing the ideal electrode array, you should consider anatomical compatibility and surgical accessibility. Your anatomy influences how well the array fits and functions, ensuring effective stimulation. Additionally, evaluate how easily your surgeon can access and implant the device safely. Balancing these factors helps select an array that maximizes performance and minimizes surgical risks, leading to better hearing outcomes tailored specifically to your unique anatomy.
Conclusion
Choosing between straight and perimodiolar electrode arrays depends on your specific needs and anatomy. Both designs aim to optimize hearing outcomes, but their success hinges on proper surgical technique and individual suitability. When you understand their differences and potential risks, you can make an informed decision. Ultimately, aligning your choice with your unique profile and hearing goals guarantees that the technology works in harmony with your ear, delivering the best possible sound experience.