Have you ever considered antibiotics as a double-edged sword? Imagine a seemingly harmless remedy that, if not used carefully, could unintentionally result in unforeseen consequences.
This delicate balance between healing and harm is precisely what we'll be exploring in our comprehensive guide on how antibiotics can cause hearing loss. As we embark on this journey, we'll uncover the intricate mechanisms behind this unexpected side effect, shedding light on the intricate interplay between medication and auditory health.
Key Takeaways
- Aminoglycosides like Gentamicin and Kanamycin can lead to sensorineural hearing loss.
- Antibiotics such as Azithromycin and Clarithromycin are linked to reversible or irreversible hearing impairment.
- Monitoring and early detection are crucial to prevent permanent hearing damage from antibiotics.
- Understanding ototoxicity mechanisms is vital for healthcare professionals to address antibiotic-induced hearing loss effectively.
Antibiotics Linked to Hearing Loss
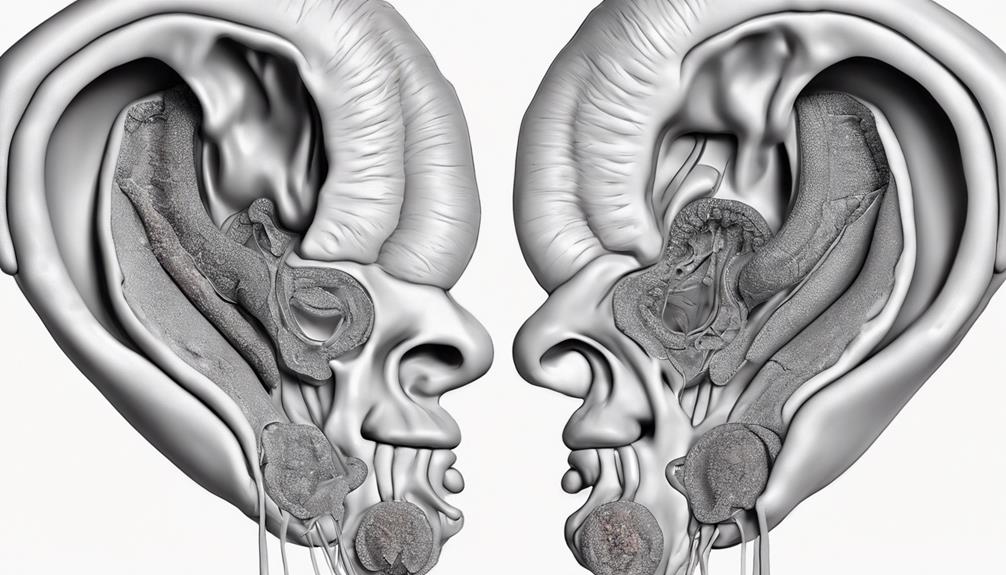
Aminoglycosides like Kanamycin, Amikacin, and Gentamicin have a well-documented association with hearing loss, particularly in vulnerable populations such as NICU infants. These antibiotics, known for their effectiveness in treating serious infections, can also have ototoxic effects on the inner ear. NICU infants receiving aminoglycosides face a higher risk, around 2-4%, of developing hearing loss compared to full-term infants. It's crucial to monitor these infants closely for any signs of hearing impairment due to aminoglycoside exposure.
While antibiotics like Azithromycin and Clarithromycin are generally considered safe, they too have been linked to hearing loss. In cases where infections cause inflammation, the risk of aminoglycoside-induced hearing loss can increase. Approximately 480,000 babies are at risk of hearing loss each year due to exposure to aminoglycoside antibiotics. Understanding the potential ototoxicity of these antibiotics is essential in managing the risks associated with their use, especially in vulnerable populations like infants.
Aminoglycosides and Hearing Loss
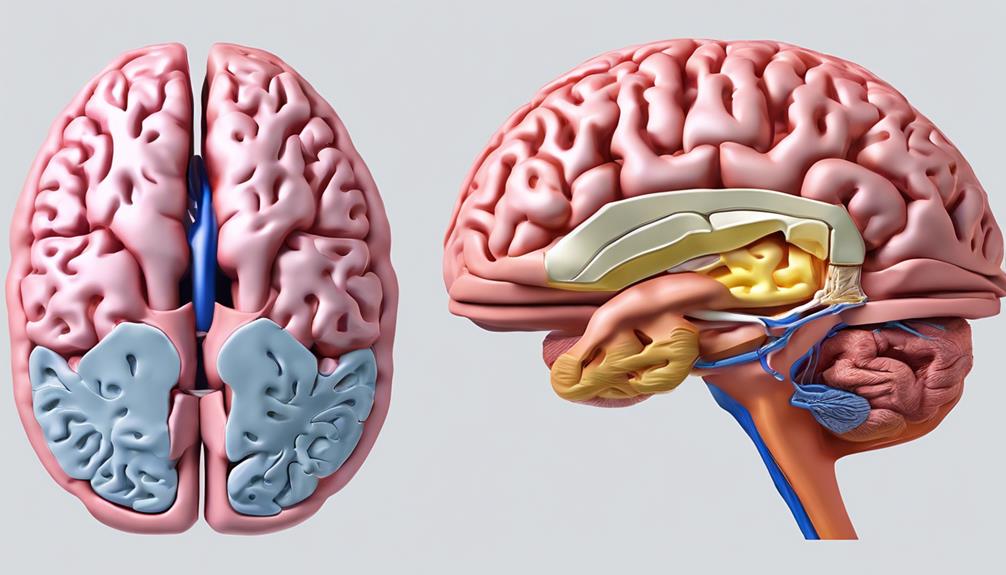
In the realm of antibiotic treatment, the impact of certain medications on hearing abilities is a crucial consideration that demands close attention. Aminoglycosides, such as gentamicin and neomycin, are potent antibiotics known to cause sensorineural hearing loss, leading to profound and permanent hearing impairment.
The ototoxic effects of aminoglycosides primarily result from inner ear sensory hair cell death, affecting the transmission of sound signals to the brain. Notably, the rate of hearing loss in NICU babies who receive aminoglycosides is significantly higher at 2-4% compared to 0.1-0.3% in full-term infants.
While aminoglycosides are vital for treating severe infections, the risk of antibiotic-induced hearing loss must be carefully monitored to prevent permanent damage. Understanding the mechanisms of ototoxicity associated with aminoglycosides is essential for healthcare professionals to mitigate the potential for profound hearing impairment in vulnerable patient populations.
Types of Antibiotic-Induced Hearing Loss
When considering antibiotic-induced hearing loss, various types of antibiotics have been associated with either reversible or irreversible impairment in auditory function. Aminoglycosides like gentamicin and neomycin are common culprits known for causing sensorineural hearing loss. Antibiotics such as azithromycin and clarithromycin have been linked to both reversible and irreversible hearing impairment. Vancomycin, often used for serious infections, may induce hearing loss, particularly in individuals with kidney issues. Certain antibiotics like kanamycin and amikacin can lead to profound and permanent hearing loss. Infection-related inflammation can heighten the risk of aminoglycoside-induced hearing loss in patients receiving these antibiotics.
| Antibiotic Type | Hearing Loss Effect | Reversibility |
|---|---|---|
| Aminoglycosides | Sensorineural | Variable |
| Azithromycin | Reversible or irreversible | Variable |
| Vancomycin | Hearing loss with kidney issues | Variable |
Diagnosing Antibiotic-Related Hearing Loss

Diagnosing antibiotic-related hearing loss involves a thorough review of the individual's medical history and current medications to identify potential factors contributing to auditory impairment. Ototoxicity, a condition where certain medications cause hearing damage, can manifest as symptoms like tinnitus (ringing in the ears) and vertigo.
Auditory tests such as pure tone audiometry and speech discrimination testing play a crucial role in diagnosing antibiotic-induced hearing loss. Early detection through comprehensive evaluations is key to preventing long-term damage from these medications.
During the diagnostic process, healthcare providers may explore the possibility of antibiotic-related hearing issues based on the presence of these symptoms and the patient's medical history. If antibiotic-induced hearing loss is confirmed, treatment options may include medications, surgery, or the use of hearing aids, tailored to the severity of the condition.
Through diligent assessment and intervention, individuals can better manage antibiotic-related hearing loss and improve their quality of life.
Prevention of Drug-Induced Ototoxicity
To prevent drug-induced ototoxicity, it is crucial to carefully select and monitor the use of medications known to cause hearing damage. When dealing with ototoxic antibiotics or drugs, several prevention strategies can be implemented.
Prevention Strategies for Drug-Induced Ototoxicity:
| Prevention Measures | Key Actions |
|---|---|
| Dosage Monitoring | Use the lowest effective dosage |
| Hearing Measurement | Measure hearing before and during treatment |
| Renal Compromise Consideration | Closer monitoring for renal-compromised patients |
| Minimizing Exposure | Avoid unnecessary exposure to ototoxic medications |
Additionally, it is essential to monitor medication levels closely, especially when patients are on multiple ototoxic medications or have renal compromise. By following these preventive measures, the risk of experiencing drug-induced ototoxicity can be minimized, ensuring better overall patient outcomes.
Frequently Asked Questions
How Do Antibiotics Cause Hearing Loss?
We know antibiotics, like aminoglycosides, can cause hearing loss. They damage inner ear sensory hair cells, primarily inducing cell death. Research delves into the molecular events and transport pathways involved.
Intracellular targets, including mitochondrial ribosomes, are being studied for their role in hearing loss. Understanding these mechanisms is crucial in preventing antibiotic-induced hearing deficits.
How Long Does Muffled Hearing Last After Antibiotics?
When antibiotics leave us with muffled hearing, the duration can vary from a few days to several weeks. Factors like the specific antibiotic and individual response play a role in this timeframe.
Recovery hinges on inner ear damage and overall health. Certain antibiotics, like gentamicin, may prolong muffled hearing even after treatment ends.
If the issue persists, it's wise to consult a healthcare provider for guidance on next steps.
What Are Five Common Medications That Are Potentially Ototoxic and May Cause Hearing Loss?
Five common medications that may cause hearing loss are:
- Aminoglycosides like gentamicin and neomycin
- Azithromycin
- Clarithromycin
- Ketoconazole
- Minocycline
- Ritonavir
These drugs have been associated with ototoxicity and can lead to varying degrees of hearing impairment.
It's crucial to be aware of the potential risks these medications pose to our hearing health and to consult with healthcare professionals if experiencing any auditory issues while on these treatments.
Which of the Following Antibiotic Is Associated With Ototoxicity and Hearing Loss?
When it comes to antibiotics linked to hearing loss, one that stands out is Aminoglycosides. These meds, like Gentamicin, Amikacin, and Neomycin, have a notorious reputation for causing ototoxicity and impairing hearing.
Their impact can be significant, especially in vulnerable populations like NICU infants. The risk of hearing loss is higher with these antibiotics, emphasizing the crucial need for vigilant monitoring to safeguard against irreversible damage.
Conclusion
In conclusion, antibiotics can indeed have a detrimental impact on our hearing health. It's crucial for us to be vigilant and proactive in monitoring our hearing while taking these medications.
Remember, our ears are precious and fragile – like delicate glass ornaments, they require careful protection and attention.
Stay informed, stay aware, and prioritize your auditory well-being.