A recent study on children who undergo ear tube surgery revealed that while the procedure effectively reduces ear infections and improves middle ear ventilation, there is a notable occurrence of temporary hearing loss post-operation.
This phenomenon raises intriguing questions about the mechanisms at play and the implications for patients' auditory health.
Understanding how ear tubes can induce such a temporary hearing impairment is crucial for healthcare providers and individuals considering this common intervention.
Key Takeaways
- Ear tubes can induce a sensorineural hearing loss component of 3 to 4 dB.
- Structural changes in the tympanic membrane impact sound conduction post-insertion.
- Multiple tube placements can worsen hearing loss, necessitating careful monitoring.
- Managing fluid drainage and infections post-surgery is crucial for preserving hearing function.
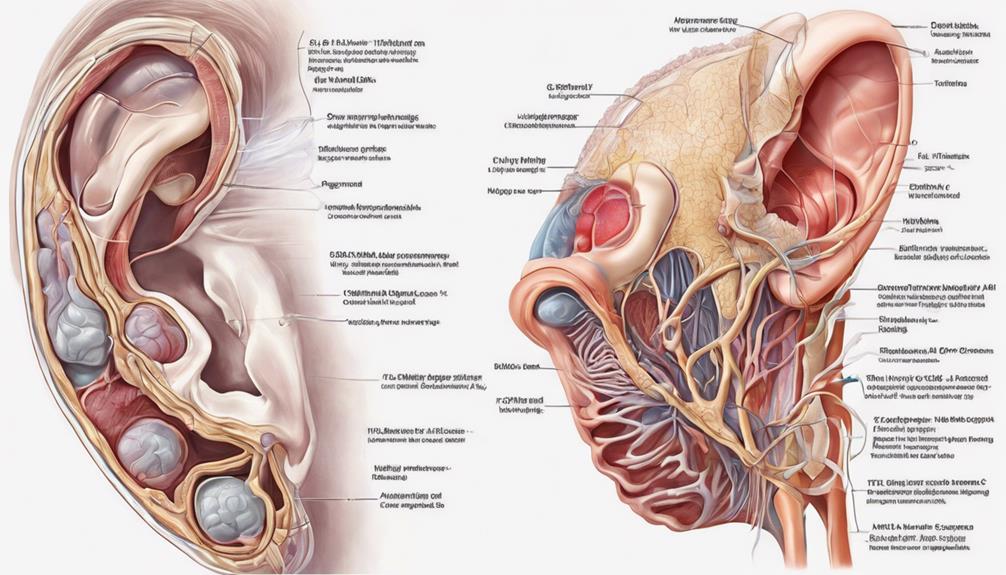
Understanding Ear Tube Functionality
When considering the functionality of ear tubes, it's crucial to understand how they impact the tympanic membrane, potentially leading to temporary hearing loss.
Ear tubes, also known as ventilation tubes, are inserted into the eardrum to alleviate middle ear infections and restore proper ventilation. However, this insertion can cause structural changes in the tympanic membrane, affecting its ability to transmit sound waves effectively.
Studies have revealed that young adults may experience a mean persistent hearing loss of approximately 5 to 10 dB after the placement of these tubes, with a sensorineural component contributing around 3 to 4 dB to this loss.
Furthermore, the causal relationship between ear tube insertion and hearing loss is rooted in the alterations that occur in the tympanic membrane post-insertion. It's essential to note that repeated insertions of ear tubes can exacerbate the deterioration of hearing, underscoring the importance of monitoring patients who undergo multiple procedures to mitigate the risk of further temporary hearing impairment.
Mechanism of Temporary Hearing Impairment

Upon the insertion of ear tubes, a notable mechanism of temporary hearing impairment emerges, elucidating the impact on auditory function through structural changes in the tympanic membrane. The process involves several key factors:
- Sensorineural Component: A temporary sensorineural component of 3 to 4 dB is linked to the insertion of ventilation tubes, contributing to the overall hearing loss experienced.
- Tympanic Membrane Changes: Structural alterations in the tympanic membrane play a critical role in the relationship between ear tube insertion and temporary hearing impairment, affecting sound conduction.
- Repeated Insertions: Multiple insertions of ear tubes can lead to a more significant deterioration in hearing compared to a single insertion, highlighting the importance of monitoring and managing repeated procedures.
- Outcome in Healthy Children: While ear tubes may cause temporary hearing impairment, studies suggest that in most cases involving healthy children, the effects resolve after tube removal, with no lasting impact on auditory function.
Factors Contributing to Hearing Loss
An essential consideration in understanding the factors contributing to hearing loss post-ear tube insertion involves the intricate interplay of structural changes in the tympanic membrane and their impact on auditory function. Ear tube insertion, often done to address recurrent otitis media or otitis media with effusion, can result in temporary hearing loss due to the presence of fluid in the middle ear. This fluid disrupts the normal sound conduction process, leading to a decrease in hearing acuity. Additionally, Eustachian tube dysfunction, commonly seen in individuals with middle ear infections, can exacerbate the issue by impairing the equalization of pressure in the middle ear.
Furthermore, the sensorineural component of hearing loss following tube insertion can also contribute to the overall decrease in hearing sensitivity. While this sensorineural hearing loss is typically mild, repeated tube insertions may lead to a cumulative effect, resulting in more significant long-term effects on hearing. Understanding these factors is crucial in managing hearing issues post-ear tube surgery effectively.
Managing Hearing Issues Post Ear Tube Surgery

To effectively manage hearing issues following ear tube surgery, regular monitoring and prompt intervention are essential components of post-operative care. After the procedure, it's crucial to focus on proper post-surgery care to optimize hearing improvement and minimize complications.
Here are key steps to manage hearing problems post ear tube surgery:
- Monitor Middle Ear Pressure: Regularly check the middle ear pressure to ensure proper functioning and prevent any discomfort.
- Manage Fluid Drainage: Keep a close watch on fluid drainage from the ear to prevent infections and maintain optimal hearing levels.
- Use Antibiotic Ear Drops: In case of post-surgery infections, promptly treat them with antibiotic ear drops to avoid any further hearing issues.
- Attend Follow-Up Appointments: Regularly attend follow-up appointments for hearing tests and assessments to track progress and address any concerns promptly.
Long-term Effects and Prognosis
After addressing immediate post-operative care following ear tube surgery, understanding the potential long-term effects and prognosis becomes crucial in managing any persistent hearing issues. Children who undergo ventilation tube insertion may experience a mean persistent hearing loss of 5 to 10 dB at the group level. This hearing loss can have a sensorineural component of 3 to 4 dB.
Structural changes in the tympanic membrane play a crucial role in the relationship between tube insertion and hearing loss. It's noted that multiple tube insertions can result in more significant deterioration of hearing compared to a single insertion.
The long-term effects of ventilation tube insertion may lead to poorer hearing outcomes in young adults, emphasizing the importance of monitoring and managing any ongoing hearing issues. Understanding these potential long-term effects is essential for healthcare providers to provide appropriate care and interventions to optimize the prognosis for individuals with ear tubes.
Frequently Asked Questions
Can Having Tubes Put in Your Ears Cause Hearing Loss?
Yes, having tubes put in your ears can cause temporary hearing loss. The insertion of ear tubes can lead to a mean persistent hearing loss of 5 to 10 dB in young adults. This loss is primarily due to a sensorineural component of approximately 3 to 4 dB.
Structural changes in the tympanic membrane play a key role in causing this temporary hearing impairment. Repeated tube insertions may exacerbate hearing deterioration compared to a single insertion.
Can Fluid in Ear Cause Temporary Hearing Loss?
Fluid in the ear can indeed cause temporary hearing loss. When the ear is filled with fluid, sound transmission through the middle ear is disrupted, impacting our ability to hear clearly.
This common issue, particularly in children with conditions like otitis media with effusion, can be alleviated with ear tubes. These tubes help drain the fluid and equalize pressure, leading to rapid improvement in hearing function.
What Are the Long Term Side Effects of Getting Tubes in Your Ears?
When considering the long-term effects of getting tubes in our ears, it's important to acknowledge potential risks. Inserting ear tubes can lead to an average persistent hearing loss of 5 to 10 dB in young adults. This hearing loss is usually linked to structural changes in the tympanic membrane caused by the insertion.
Repeated tube insertions may worsen hearing loss compared to a single insertion, but scarring from the procedure generally has minimal impact on hearing abilities.
Can a Blocked Eustachian Tube Cause Temporary Hearing Loss?
Yes, a blocked Eustachian tube can indeed cause temporary hearing loss. When the Eustachian tube is blocked, fluid can accumulate in the middle ear, affecting the proper vibration of the eardrum and hindering sound conduction.
This issue is commonly observed in children with ear infections or allergies. Fortunately, this type of hearing loss is reversible once the underlying cause, such as congestion or infection, is addressed promptly.
Conclusion
In conclusion, ear tubes can lead to temporary hearing loss due to structural changes in the ear following insertion.
It's important to note that young adults may experience an average persistent hearing loss of about 5 to 10 dB after ventilation tube insertion.
This statistic highlights the potential impact of ear tubes on hearing ability and emphasizes the importance of monitoring and managing any hearing issues post-surgery for optimal outcomes.