When studying how medications impact our health, it is crucial to explore the connection between furosemide and hearing loss. By examining how this commonly prescribed diuretic can impact our ability to hear, we can better understand the complexities of drug-induced ototoxicity.
As we navigate the intricate pathways through which furosemide affects our hearing, it becomes evident that awareness of these mechanisms is essential for both healthcare professionals and patients alike. Stay tuned to uncover the intricate details surrounding furosemide's potential ototoxic effects and the significance of proactive management strategies in mitigating harm.
Key Takeaways
- Furosemide disrupts cochlear function, impacting auditory abilities.
- Risk factors like renal failure heighten susceptibility to furosemide-induced hearing loss.
- Monitoring drug levels and serum albumin is crucial for patient safety.
- Timely detection of ototoxicity symptoms and collaboration between healthcare providers are essential.
Ototoxic Effects of Furosemide
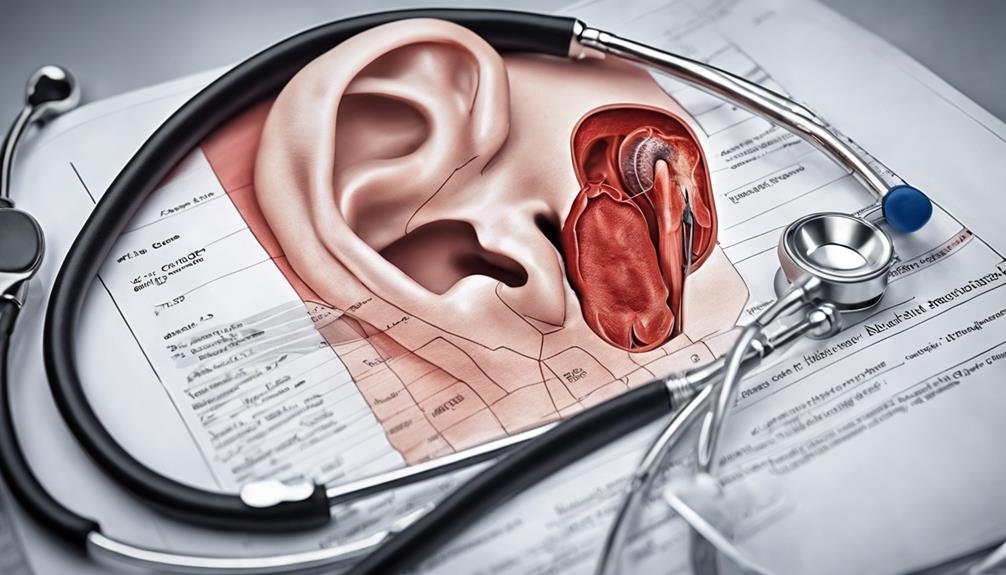
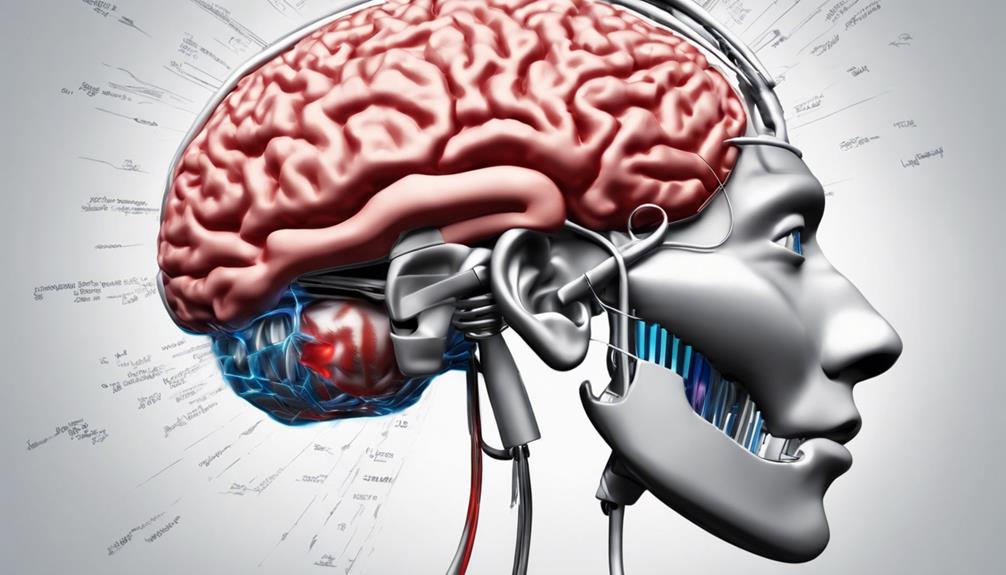
When considering the ototoxic effects of furosemide, it becomes evident that this diuretic medication induces specific pathological changes in the cochlea, thereby affecting auditory function. Furosemide's impact on the cochlea is multifaceted, leading to ototoxicity through various mechanisms. One crucial effect is the disruption of the endolymphatic potential, crucial for normal cochlear function. Additionally, furosemide interferes with the cochlear microphonic potential, essential for sound transduction.
Moreover, furosemide compromises the integrity of the blood-cochlea barrier, allowing harmful substances to penetrate the cochlear compartments. This breach can result in temporary pathological changes and edema in the stria vascularis and the cochlear lateral wall. Furthermore, furosemide's interference with strial adenylate cyclase, Na+/K+-ATPase, and the Na-K-2Cl cotransporter in the stria vascularis contributes to its ototoxic effects. These disruptions lead to rapid reductions in cochlear action potential amplitude, further impacting auditory function.
Understanding these intricate mechanisms is crucial for managing furosemide-induced hearing loss effectively.
Mechanisms of Hearing Loss
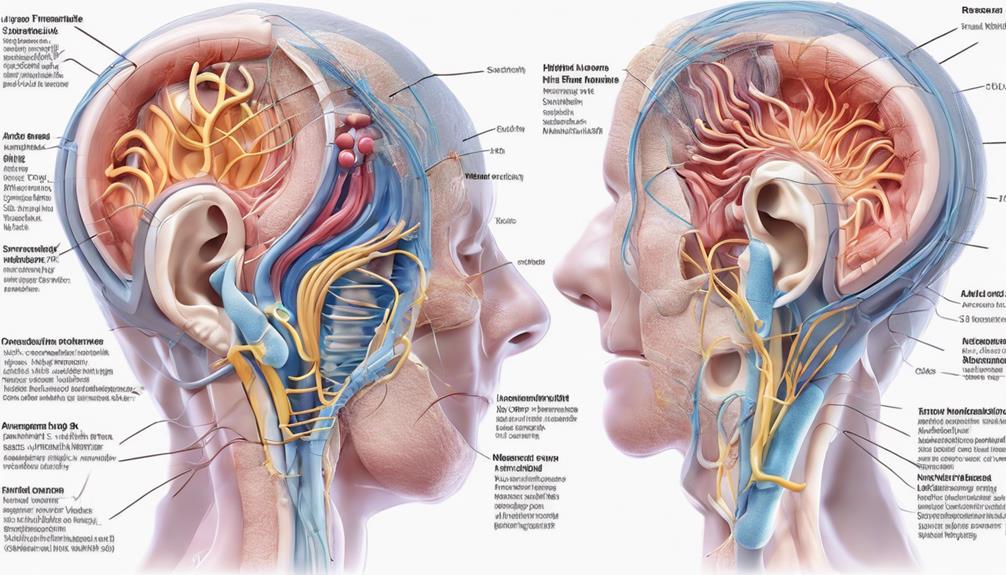
Furosemide-induced hearing loss manifests through intricate mechanisms involving edema and cystic changes in the stria vascularis of the cochlea, affecting critical auditory functions. Loop diuretics like furosemide disrupt the endocochlear potential and cochlear microphonic potential, contributing to hearing impairment. The stria vascularis plays a vital role in maintaining the endocochlear potential necessary for proper hearing function. When furosemide interferes with this delicate balance, cochlear damage ensues, leading to hearing loss.
Moreover, individuals with renal or hepatic failure are at an increased risk of experiencing furosemide-induced ototoxicity due to impaired drug clearance mechanisms. Prolonged exposure to furosemide can exacerbate the injury to the stria vascularis, amplifying the severity of hearing impairment. Factors such as high drug concentrations, low serum albumin levels, or pre-existing hepatic conditions can further heighten the susceptibility to furosemide-induced hearing loss. Understanding these mechanisms is crucial for healthcare professionals to monitor and mitigate the potential ototoxic effects of furosemide on their patients' hearing health.
Risk Factors for Ototoxicity
Patients at risk of furosemide-induced ototoxicity exhibit specific factors that heighten their susceptibility to cochlear damage. Some of these risk factors include:
- Low Serum Albumin Levels: Patients with low serum albumin levels are more prone to experiencing ototoxic effects from furosemide. This is an important consideration when prescribing loop diuretics to individuals with compromised albumin levels.
- High Plasma Protein Binding: Furosemide's high plasma protein binding can lead to higher drug concentrations in the body, increasing the likelihood of ototoxicity. Monitoring drug levels in patients with altered protein binding capacity is crucial.
- Asymmetric Hearing Loss: Ototoxic effects of furosemide can manifest as asymmetric hearing loss, where one ear is more affected than the other. Recognizing this pattern underscores the importance of regular monitoring and early intervention to prevent further hearing deterioration.
Understanding these risk factors can aid healthcare providers in identifying patients who may be more vulnerable to furosemide-induced ototoxicity.
Mitigating Furosemide-Induced Hearing Loss

To address the mitigation of hearing loss induced by furosemide, understanding the factors contributing to cochlear damage in high-risk patients with hepatic or renal failure is essential. Monitoring drug concentrations in individuals receiving furosemide is crucial to prevent ototoxic effects. Patients with lower serum albumin levels are at higher risk of experiencing the damaging effects of furosemide on hearing. Prolonged exposure to furosemide can escalate the risk and severity of injury to the cochlear structures. In cases of severe hearing loss resulting from furosemide ototoxicity, cochlear implantation may offer a potential solution. Below is a table summarizing key points to consider in mitigating furosemide-induced hearing loss:
| Factor | Importance | Action Needed |
|---|---|---|
| Serum Albumin Levels | Higher risk with lower levels | Monitor levels regularly |
| Prolonged Furosemide Exposure | Increases injury risk to cochlea structures | Consider dosage adjustments or alternative meds |
| Cochlear Implantation | Option for severe hearing loss cases | Evaluate candidacy and discuss with specialists |
Importance of Regular Monitoring
Regular monitoring of individuals prescribed with furosemide is imperative for the timely detection of any potential signs of ototoxicity. Patients on furosemide should undergo regular hearing tests to evaluate changes in auditory function. Symptoms such as tinnitus, vertigo, or hearing loss must be closely monitored for early intervention.
Seeking consultation with an audiologist or otolaryngologist for specialized assessment is highly recommended. These professionals can provide in-depth evaluations to detect any subtle changes in auditory health that may indicate ototoxicity.
Through vigilant monitoring, healthcare providers can promptly identify any adverse effects of furosemide on hearing and take necessary actions to mitigate further damage. Regular check-ups and assessments can help in making timely adjustments to medication dosage or exploring alternative treatment options to prevent irreversible hearing loss.
Frequently Asked Questions
How Does Lasix Affect Your Ears?
Lasix, also known as furosemide, affects the ears by inducing hearing loss through damage to the cochlea's stria vascularis. This medication can harm inner and outer hair cells, potentially leading to tectorial membrane collapse.
Prolonged exposure to Lasix exacerbates injury in the stria vascularis, increasing the risk of hearing impairment. In cases of ototoxicity from Lasix, patients with uneven hearing loss might benefit from cochlear implants for auditory function restoration.
Do Water Pills Cause Hearing Loss?
Water pills, or diuretics, can indeed cause hearing loss. The mechanism involves disruption of crucial cochlear functions, impacting the ability to detect sound.
This effect can be detrimental and warrants caution when using such medications. Understanding the potential risks and working closely with healthcare providers can help mitigate these concerns.
It's essential to prioritize hearing health and seek appropriate guidance when considering medications that may impact it.
How Does Furosemide Cause Tinnitus?
Furosemide can lead to tinnitus through its impact on the cochlea, altering endolymphatic potential and disrupting the blood-cochlea barrier. This disruption allows harmful substances to enter the cochlea, triggering tinnitus.
Research shows that furosemide treatment can cause temporary damage to the cochlear lateral wall, exacerbating tinnitus symptoms.
Understanding these mechanisms is vital for managing tinnitus and preventing further hearing loss.
Which Drug Group May Increase the Risk of Ototoxicity Associated With Furosemide?
We know that certain drug groups can heighten the risk of ototoxicity linked to furosemide. Factors like drug concentration and patient health status play a role.
Patients on thiazide diuretics or furosemide should be aware of this potential complication. It's crucial for healthcare providers to monitor for signs of hearing loss in these individuals.
Understanding these risks is vital for ensuring patient safety and well-being.
Conclusion
In conclusion, it's crucial for healthcare providers to stay vigilant when prescribing furosemide and other ototoxic drugs.
By understanding the mechanisms behind furosemide-induced hearing loss and implementing regular monitoring, we can proactively prevent irreversible damage to the cochlea.
Remember, an ounce of prevention is worth a pound of cure when it comes to protecting our patients' hearing health.
Stay informed, stay proactive, and together, we can make a difference in preventing ototoxicity.