As we delve into the intricate connection between stroke and hearing loss, it is evident that the impact of vascular events on hearing abilities can be substantial.
Imagine the implications of this relationship on individuals striving to navigate everyday conversations and maintain their quality of life.
Understanding how stroke can lead to hearing impairments opens a door to a realm of crucial insights that could potentially revolutionize the care provided to those affected.
Let's explore the depths of this connection, unveiling the complexities that lie beneath the surface.
Key Takeaways
- Stroke impacts auditory pathways, leading to hearing dysfunction.
- Thorough assessments post-stroke are crucial for identifying hearing loss.
- Understanding mechanisms aids in managing post-stroke hearing impairment.
- Treatment options include hearing aids, cochlear implants, and auditory training.
Stroke and Hearing Loss Relationship
Stroke commonly causes hearing loss by affecting various levels of the auditory pathway. The intricate relationship between stroke and hearing loss underscores the necessity for thorough auditory assessments post-stroke.
Research indicates a high incidence of auditory dysfunction following a stroke, emphasizing the need for a comprehensive evaluation to address potential deficits effectively. Auditory-processing deficits, although frequently overlooked, can have profound implications for patient communication abilities and overall outcomes.
By recognizing and addressing these hearing impairments promptly, healthcare professionals can significantly enhance patient communication and quality of life. Comprehensive assessment tools play a crucial role in identifying the extent of hearing loss and auditory challenges in stroke survivors.
Understanding the impact of stroke on the auditory system is paramount to implementing targeted interventions that can mitigate communication barriers and improve patient outcomes in the long term.
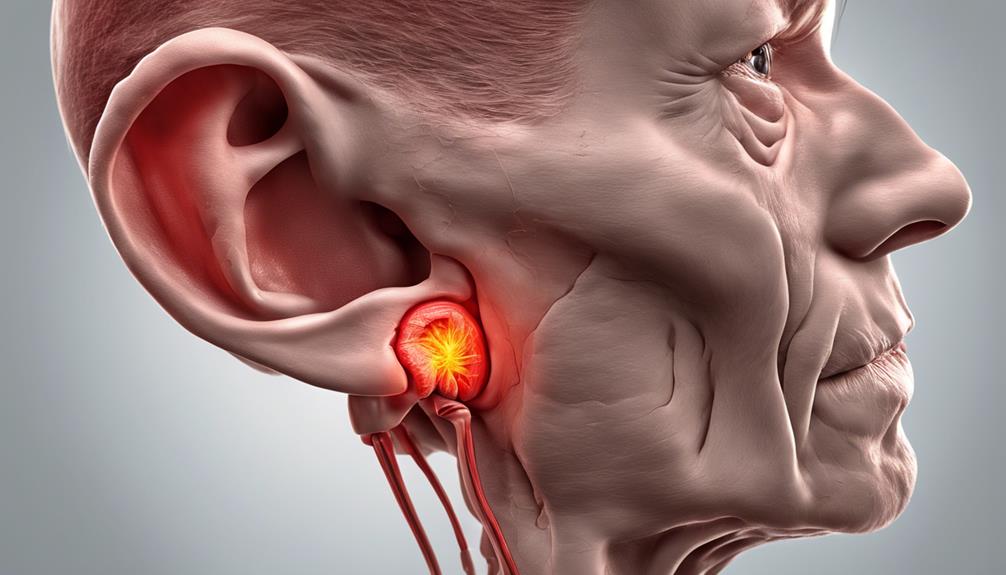
Mechanisms of Hearing Impairment Post-Stroke

Exploring the intricate neural pathways involved in auditory processing post-stroke reveals the complex mechanisms underlying hearing impairment in affected individuals. When stroke impacts the auditory pathway, it can lead to deficits in hearing reception and perception, significantly affecting communication abilities.
The underdocumented auditory-processing deficits post-stroke can have a profound impact on patient outcomes, emphasizing the importance of comprehensive auditory assessments in stroke survivors. Stroke affecting the outer brain stem can also play a crucial role in hearing loss, highlighting the need for early recognition and intervention.
Understanding the pathophysiological mechanisms behind auditory deficits post-stroke is essential for developing effective management strategies tailored to individual needs. By addressing the specific challenges in auditory function caused by stroke, healthcare professionals can better support patients in their recovery journey and enhance their quality of life.
Recognizing Early Signs of Hearing Loss
Recognizing early signs of hearing loss post-stroke involves closely monitoring for sudden sensorineural hearing loss (SSNHL) symptoms and seeking prompt medical evaluation. SSNHL can manifest as a sudden, significant hearing impairment in one ear, with individuals waking up to this change or noticing a gradual decline in hearing over time following a stroke.
SSNHL is characterized by a decrease of at least 30 decibels in three consecutive frequencies and can occur within three days. Various factors such as vascular occlusion, viral infections, ruptured inner ear membranes, tumors, and autoimmune diseases can contribute to sudden hearing loss post-stroke.
To detect hearing loss early, it's crucial to monitor for signs of impending stroke, undergo comprehensive neurological exams, and schedule a hearing assessment promptly. By staying vigilant and proactive in monitoring auditory impairment post-stroke, individuals can enhance their chances of early detection and timely intervention for improved management of hearing issues.
Treatment Options for Stroke-Related Hearing Issues

In managing stroke-related hearing issues, a range of treatment options such as hearing aids, cochlear implants, auditory training, and speech therapy can be considered. These interventions aim to enhance communication, restore auditory function, and improve the overall quality of life for individuals affected by stroke-induced hearing deficits. When developing a comprehensive treatment plan, a multidisciplinary approach involving audiologists, otolaryngologists, and speech-language pathologists is crucial. Customized hearing rehabilitation plans tailored to individual needs and preferences play a key role in optimizing outcomes for stroke patients experiencing hearing problems. Regular follow-up appointments and adjustments to treatment plans are essential to address evolving auditory needs and ensure optimal hearing outcomes post-stroke.
- Hearing Aids: These devices amplify sound to improve hearing ability.
- Cochlear Implants: Surgically implanted devices that directly stimulate the auditory nerve.
- Auditory Training and Speech Therapy: Programs designed to enhance listening skills and improve speech understanding.
Tips for Protecting Hearing Health Post-Stroke
To safeguard hearing health following a stroke, prioritizing regular assessments to monitor changes in auditory function is essential. These assessments can help detect any alterations in hearing abilities promptly, allowing for timely intervention. Implementing lifestyle modifications such as focusing on cardiovascular health and avoiding exposure to loud noises can also contribute to protecting hearing post-stroke. Additionally, engaging in auditory rehabilitation programs and utilizing hearing aids or assistive devices may enhance communication outcomes for individuals experiencing hearing loss after a stroke. It is crucial to seek immediate medical attention for any sudden changes in hearing, as addressing these issues promptly can prevent further complications. Educating caregivers and healthcare providers about the impact of hearing loss post-stroke is vital in ensuring comprehensive support and effective management strategies for affected individuals.
| Hearing Health Tips Post-Stroke | |
|---|---|
| Regular Hearing Assessments | Monitor changes in auditory function to detect issues early. |
| Lifestyle Modifications | Focus on cardiovascular health and avoid loud noise exposure. |
| Auditory Rehabilitation Programs | Engage in programs to improve communication outcomes. |
| Hearing Aids & Assistive Devices | Utilize devices to enhance hearing abilities and communication. |
| Prompt Medical Attention | Seek immediate help for sudden changes in hearing to address issues early. |
Frequently Asked Questions
How Does a Stroke Cause Hearing Loss?
When a stroke occurs, it can impact the auditory pathway within the brain, leading to hearing loss. Lesions in the auditory cortex or brainstem can cause deficits in hearing reception and perception.
The prevalence of hearing loss post-stroke underscores the influence of vascular issues on auditory function. Different stroke types like AICA or PICA can result in specific hearing loss patterns.
Understanding how strokes disrupt the auditory system is vital for diagnosing and managing post-stroke hearing deficits.
Can Hearing Loss From Stroke Be Reversed?
Yes, hearing loss from a stroke can be reversed in some cases through prompt medical intervention and rehabilitative measures. Statistics show that early diagnosis and treatment of the underlying cause post-stroke can significantly improve recovery chances.
Rehabilitation programs focusing on auditory training and therapy play a crucial role in enhancing communication and hearing abilities following a stroke. The extent of reversal varies based on the severity of damage to the auditory pathways.
What Is the Most Common Cause of Hearing Loss?
The most common cause of hearing loss is sensorineural hearing loss (SNHL), affecting the inner ear or auditory nerve. SNHL can stem from factors like aging, exposure to loud noise, genetics, and specific medications.
Conductive hearing loss, related to outer or middle ear issues, and mixed hearing loss, combining sensorineural and conductive elements, are also prevalent.
Understanding these distinctions is vital for tailoring appropriate treatment strategies based on the root cause of the hearing impairment.
What Can Cause Sudden Hearing Loss?
When sudden hearing loss strikes, various factors like vascular issues, infections, membrane ruptures, tumors, and autoimmune diseases can be culprits. This condition typically affects one ear, causing a rapid loss of at least 30 dB across three frequencies.
The inner ear's susceptibility to ischemia plays a role in this sudden impairment, with cochlear infarctions sometimes being involved. The onset can be rapid, waking individuals up or gradually developing over three days.
Conclusion
In conclusion, understanding the intricate relationship between stroke and hearing loss is crucial for improving patient outcomes. Like a symphony conductor guiding each instrument to create harmonious music, early detection and management of hearing deficits post-stroke can orchestrate better communication and quality of life for individuals.
By recognizing the signs, exploring treatment options, and protecting hearing health, we can strive towards a more harmonious future for stroke survivors.