When assessing the advantages and disadvantages of medication, it is important to consider the intricate impact furosemide can have on auditory health. Understanding how furosemide can cause hearing loss requires a thorough examination of its mechanisms and potential consequences.
As we navigate through the complexities of ototoxicity induced by this commonly prescribed diuretic, a deeper awareness of its effects on auditory function unveils a compelling narrative that beckons us to unravel the mysteries lurking within its pharmacological pathways.
Key Takeaways
- Furosemide disrupts cochlear blood flow, leading to hearing loss.
- Rapid decrease in endocochlear potential occurs due to furosemide.
- Interference with ion transport mechanisms in the cochlea contributes to ototoxicity.
- Monitoring for auditory symptoms is crucial to understand furosemide's impact on hearing.
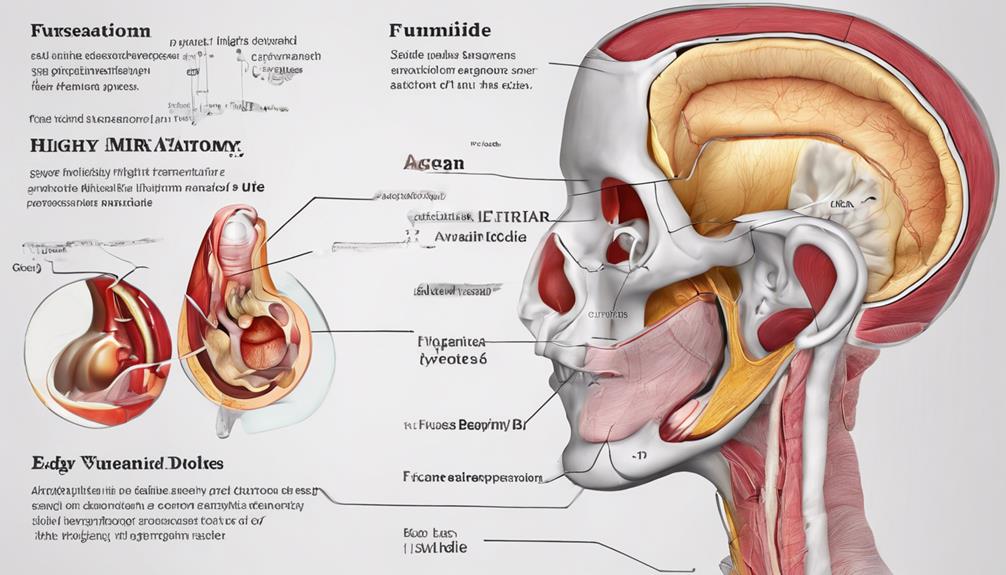
Mechanisms of Furosemide-Induced Hearing Loss
Furosemide induces hearing loss through its disruption of blood flow in the cochlear lateral wall, resulting in rapid reductions in endocochlear potential. This ototoxic effect is a result of furosemide's action as a loop diuretic, which interferes with the normal ion transport mechanisms crucial for maintaining cochlear function.
The stria vascularis, responsible for generating the endocochlear potential essential for hair cell function, experiences edema due to furosemide, leading to cochlear damage. Moreover, furosemide disrupts microcirculation in the cochlear lateral wall, impairing enzyme function and ion transport in the stria vascularis.
The alteration of the blood-cochlea barrier by furosemide further exacerbates the issue by allowing harmful substances to penetrate the cochlea, contributing to hearing loss. Understanding these intricate pathways sheds light on the complex interplay of factors that underlie furosemide-induced ototoxicity, emphasizing the importance of monitoring patients on loop diuretics for potential cochlear side effects.
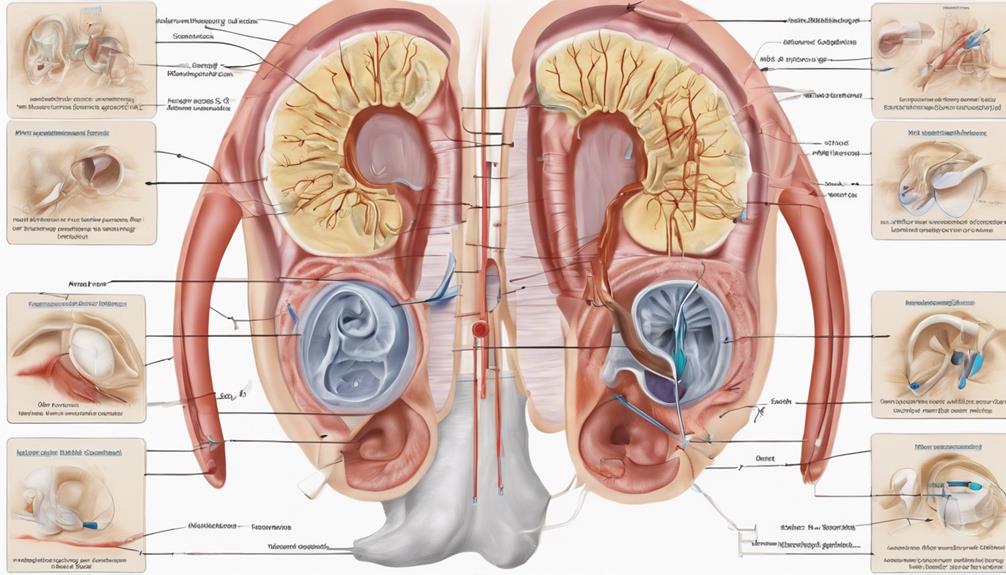
Risk Factors for Furosemide Ototoxicity
High doses, prolonged use, preexisting hearing impairment, and concomitant administration of other ototoxic medications are among the identified risk factors for the development of ototoxicity associated with furosemide. Patients with renal impairment, especially those receiving intravenous furosemide, face an elevated risk of furosemide-induced hearing loss. Elderly individuals, particularly those with age-related hearing loss, exhibit heightened susceptibility to furosemide ototoxicity.
The concurrent use of furosemide with aminoglycoside antibiotics or platinum-containing chemotherapy agents can further increase the risk of ototoxic effects. Additionally, patients with electrolyte imbalances like hypokalemia or hypocalcemia may be more predisposed to furosemide-induced ototoxicity due to alterations in cochlear function.
Understanding these risk factors is crucial for healthcare professionals when prescribing furosemide, allowing them to monitor patients closely for signs of ototoxicity and take necessary precautions to prevent potential hearing loss complications.
Management of Furosemide-Related Hearing Loss
Early identification of symptoms such as tinnitus, vertigo, and hearing impairment is crucial in the management of furosemide-related hearing loss. Audiometric monitoring plays a vital role in detecting changes in hearing thresholds promptly. Adjusting furosemide dosages or considering alternative diuretics may help prevent further ototoxicity. Collaborating with healthcare providers to assess renal function and overall medication regimens can aid in managing furosemide-induced hearing loss effectively. Educating patients on the risks of furosemide ototoxicity and stressing the importance of regular hearing evaluations are essential components of successful management strategies.
- Audiometric Monitoring: Regular assessments to monitor changes in hearing thresholds.
- Medication Adjustment: Consider altering furosemide dosages or switching to alternative diuretics.
- Renal Function Assessment: Collaborate with healthcare providers to evaluate renal function.
- Patient Education: Educate patients on the risks of furosemide ototoxicity and the importance of regular hearing evaluations.
Preventing Furosemide-Induced Hearing Damage
To prevent hearing damage induced by furosemide, close monitoring of patients before and during treatment is crucial for early detection of potential ototoxic effects. Administering furosemide at the lowest effective dose can help reduce the risk of hearing loss. Patients should be closely monitored for signs of ototoxicity, such as tinnitus or vertigo, to promptly address any emerging issues.
It's important to avoid concurrent use of other ototoxic medications with furosemide as this can exacerbate the risk of hearing damage. Patients with renal compromise require heightened monitoring when prescribed furosemide to prevent ototoxic effects. Regular hearing assessments and vigilance for any auditory symptoms are essential components of preventing furosemide-induced hearing damage.
Understanding Furosemide's Impact on Hearing
Furosemide's impact on hearing is primarily attributed to its disruption of blood flow in the cochlear lateral wall, resulting in rapid reductions in endocochlear potential. This disturbance in blood flow can lead to cochlear ischemia, affecting the delicate balance necessary for proper hearing function.
Additionally, furosemide's interference with the Na-K-2Cl cotransporter in the stria vascularis plays a crucial role in inducing hearing loss by disrupting ion reabsorption processes essential for auditory signal transduction. The cascade of events triggered by furosemide administration can ultimately result in cochlear damage, contributing to the development of ototoxicity and potential long-term hearing impairment.
Understanding the intricate mechanisms through which loop diuretics like furosemide impact the cochlea sheds light on the complexity of drug-induced hearing loss and underscores the importance of monitoring patients for signs of auditory damage.
Frequently Asked Questions
How Does Furosemide Cause Hearing Loss?
Furosemide causes hearing loss by disrupting blood flow in the cochlear lateral wall, leading to rapid reductions in endocochlear potential. Loop diuretics interfere with critical mechanisms in the cochlea, contributing to ototoxic effects.
Studies suggest that furosemide-induced ischemia damages the stria vascularis and cochlear lateral wall, affecting cochlear function. Furosemide increases the blood-cochlear barrier's permeability, allowing ototoxic substances to enter the cochlea and impact hearing.
Timing furosemide administration with other drugs is critical for managing cochlear damage.
How Does Lasix Affect Your Ears?
Lasix, a loop diuretic, impacts our ears by disrupting the blood-cochlea barrier and causing rapid reductions in cochlear action potential. It interferes with critical mechanisms in the stria vascularis, like Na+/K+-ATPase and the Na-K-2Cl cotransporter. This leads to edema in the epithelium of the stria vascularis and changes in cochlear barrier permeability.
Lasix can halt blood flow in the cochlear lateral wall, inducing ischemia and anoxia in the stria vascularis.
What Are the Symptoms of Furosemide Ototoxicity?
When it comes to symptoms of furosemide ototoxicity, we may experience:
- Hearing loss
- Ringing in the ears (tinnitus)
- Dizziness
This drug can impact our ability to hear high-pitched sounds, either temporarily or permanently. Some users might feel unsteady or have episodes of vertigo due to its effects.
Monitoring for ear-related issues and balance problems is essential to prevent irreversible hearing damage when using furosemide.
Is Furosemide Related to Ototoxicity?
Yes, furosemide is linked to ototoxicity.
It has been established that furosemide, a loop diuretic, can induce hearing loss by disrupting cochlear functions.
Research indicates that furosemide interferes with the cochlear microphonic potential and key processes in the stria vascularis, leading to a decrease in cochlear action potential amplitude.
Additionally, furosemide can compromise the blood-cochlea barrier, enabling harmful substances to enter the cochlea and cause damage.
Conclusion
In conclusion, the intricate interplay between furosemide and cochlear function highlights the potential risks associated with its use.
By understanding the mechanisms of furosemide-induced hearing loss, identifying high-risk patients, and implementing preventive measures, healthcare professionals can effectively manage this ototoxicity.
This comprehensive guide serves as a valuable resource for navigating the complexities of furosemide-related hearing damage, ultimately enhancing patient care and outcomes in clinical practice.