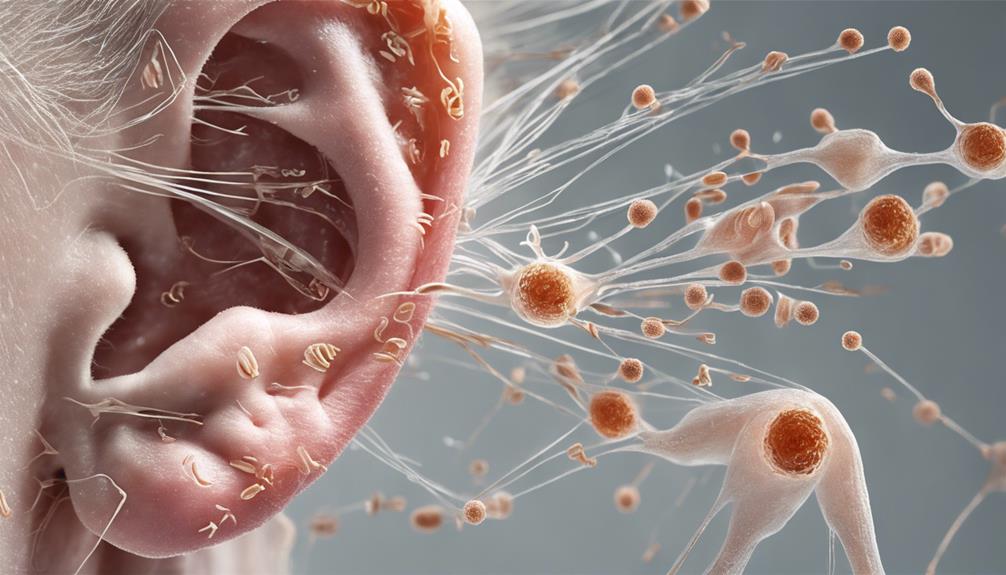
Imagine the intricate workings of the inner ear as a finely tuned mechanism, where each component plays a crucial role in the beautiful sounds we hear.
Yet, when exposed to gentamicin, this harmony can be disrupted, leading to potential harm. Understanding how this antibiotic can impact our hearing is crucial, as it unveils a world where vigilant monitoring and proactive measures can make all the difference in preserving our precious sense of sound.
Key Takeaways
- Gentamicin induces hearing loss via cochleotoxic and vestibulotoxic pathways.
- Genetic predisposition and high-dose therapy increase susceptibility to aminoglycoside-induced damage.
- Early detection through audiometric assessments and vigilant monitoring are crucial.
- Tailored interventions and dose adjustments optimize outcomes for at-risk patients.
Ototoxicity Mechanisms of Gentamicin
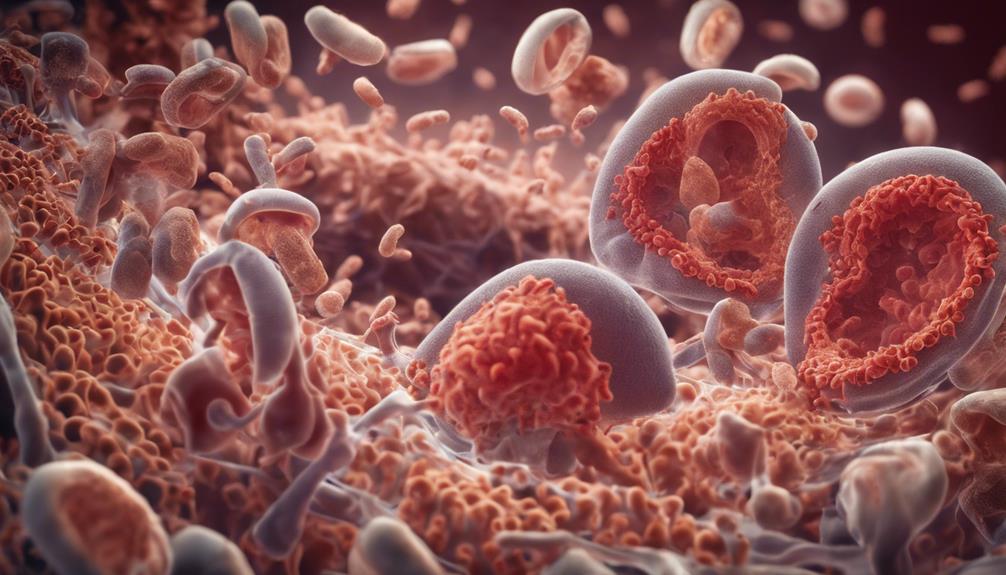
Gentamicin exerts its ototoxic effects through intricate mechanisms involving both vestibulotoxic and cochleotoxic pathways. The cochleotoxicity of gentamicin, a significant concern, leads to sensorineural hearing loss, especially in high-risk groups receiving high-dose therapy. Mitochondrial DNA mutations play a crucial role in aminoglycoside ototoxicity, predisposing individuals to hearing damage. These mutations contribute to the vulnerability of the cochlea to gentamicin-induced damage, emphasizing the need for monitoring in susceptible populations.
Additionally, the vestibulotoxic effects of gentamicin can result in unilateral hearing loss, independent of cochlear damage, highlighting the complexity of aminoglycoside ototoxicity.
Moreover, existing bioprotective mechanisms can counter the vestibulotoxic effects of gentamicin, suggesting potential avenues for mitigating ototoxicity in clinical settings. Understanding these ototoxicity mechanisms is essential for developing targeted interventions to prevent or minimize hearing damage associated with gentamicin treatment. The multifaceted nature of gentamicin-induced ototoxicity underscores the importance of tailored approaches to protect auditory function.
Risk Factors for Hearing Damage
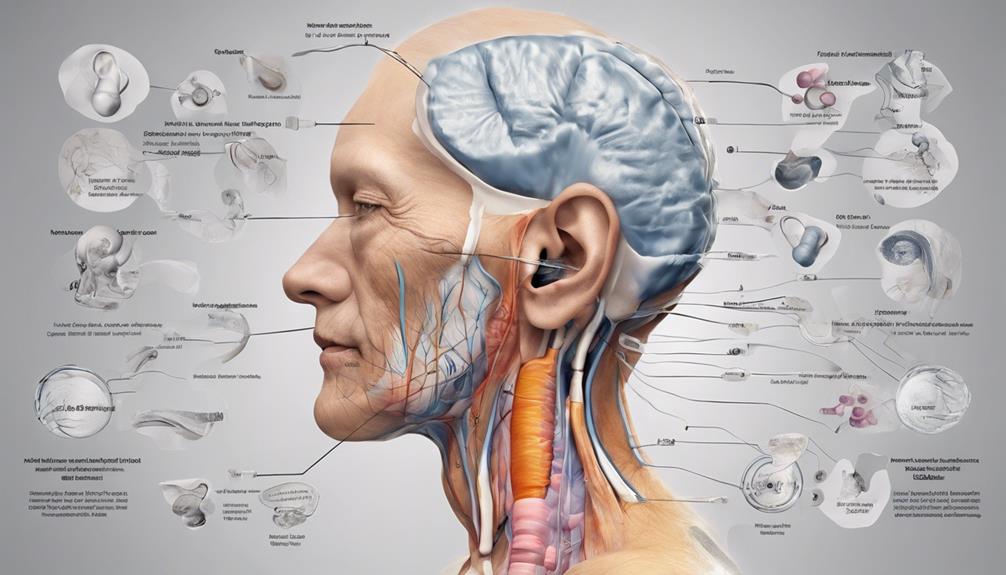
Genetic predisposition and mitochondrial gene mutations significantly influence the risk of aminoglycoside-induced hearing loss. Patients undergoing high-dose aminoglycoside therapy are particularly vulnerable to developing sensorineural hearing loss due to these factors.
Genetic predisposition, in conjunction with aminoglycoside exposure, can amplify the likelihood of ototoxicity. The potential for irreversible damage to auditory function underscores the importance of identifying individuals at higher risk. Genetic screening emerges as a valuable tool in recognizing susceptibility to aminoglycoside-induced hearing loss.
Understanding the interplay between genetic predisposition, mitochondrial gene mutations, and aminoglycoside ototoxicity is crucial in clinical practice. By recognizing these risk factors, healthcare providers can tailor interventions and monitoring strategies to mitigate the impact of aminoglycoside-induced hearing damage. Vigilance in identifying at-risk patients and implementing appropriate measures is essential in safeguarding auditory function during aminoglycoside therapy.
Monitoring Gentamicin-Induced Hearing Loss
Aminoglycoside-induced hearing damage necessitates vigilant monitoring strategies, especially focusing on high-frequency audiometric assessments for early detection of potential gentamicin-induced auditory toxicity. Audiometric monitoring plays a crucial role in identifying changes in hearing thresholds, specifically targeting the high-frequency range where gentamicin-induced ototoxicity often initially manifests. Alongside audiometric evaluations, monitoring for vestibular dysfunction symptoms is vital in patients undergoing aminoglycoside therapy. These assessments aid in the prompt recognition of any emerging issues related to gentamicin exposure, allowing for timely intervention to prevent further auditory damage. Unfortunately, there are currently no proven bioprotective agents available to mitigate the ototoxic effects of gentamicin. Therefore, regular audiometric monitoring remains the cornerstone in managing aminoglycoside-induced ototoxicity. Early detection of hearing loss and prompt cessation of aminoglycoside therapy can significantly improve the chances of recovery from gentamicin-induced hearing damage.
| Audiometric Monitoring | Importance | Notes |
|---|---|---|
| High-frequency range | Early detection | Initial site of gentamicin toxicity |
| Vestibular symptoms | Crucial assessment | Identifying potential side effects |
| Regular evaluations | Key for intervention | Monitoring treatment progression |
Minimizing Gentamicin's Impact on Hearing

To minimize the impact of gentamicin on hearing, monitoring gentamicin levels and making appropriate dose adjustments have been identified as effective strategies. Clinical data from studies comparing gentamicin exposure between individuals with hearing loss and those without have shown no significant differences in treatment parameters.
Early detection of ototoxicity through continuous monitoring and timely dose adjustments is crucial in reducing the risk of hearing loss associated with aminoglycoside antibiotics like gentamicin. Analysis of gentamicin exposure data from infants born over a specific period has provided valuable insights into strategies aimed at mitigating the impact of gentamicin on hearing.
These findings underscore the importance of vigilant monitoring and judicious management of gentamicin treatment to minimize the potential for ototoxicity and subsequent hearing loss. By incorporating these practices into clinical protocols, healthcare providers can optimize patient outcomes and enhance the safety profile of gentamicin therapy.
Safer Use of Gentamicin in Practice
In clinical practice, vigilant monitoring of gentamicin usage is essential to ensure the safe administration of the antibiotic and prevent potential ototoxic effects. Healthcare professionals must carefully monitor gentamicin levels and be prepared to adjust doses accordingly to minimize the risk of ototoxicity.
Patients with pre-existing hearing issues require special consideration when prescribing gentamicin to avoid worsening their condition. For individuals at high risk of experiencing ototoxic effects, exploring safer alternatives to gentamicin should be a priority to safeguard their hearing health.
Timely interventions play a crucial role in identifying and addressing hearing loss symptoms in patients undergoing gentamicin treatment, potentially leading to improved outcomes. Being aware of the potential ototoxic effects of gentamicin and proactively managing its usage are paramount in promoting safe practices within healthcare settings.
Frequently Asked Questions
How Does Gentamicin Cause Hearing Loss?
Gentamicin causes hearing loss by damaging sensory hair cells in the inner ear. This damage results from oxidative stress and cell death in the cochlea, disrupting mitochondrial function in hair cells and impairing energy production.
Exposure to gentamicin can lead to permanent sensorineural hearing loss that's irreversible. Inflammation can exacerbate the ototoxic effects of gentamicin on cochlear cells, increasing the risk of hearing damage.
Why Does Aminoglycosides Cause Hearing Loss?
We all know why aminoglycosides cause hearing loss. These antibiotics damage sensory hair cells in the inner ear, disrupting crucial cochlear structures.
Unfortunately, this ototoxicity is irreversible in mammals due to the lack of spontaneous hair cell regeneration. While aminoglycosides are potent against gram-negative bacteria, they come with a risk of significant and permanent hearing damage.
Healthcare professionals must grasp these effects to minimize hearing loss risks in patients.
What Does Gentamicin Do to the Inner Ear?
Gentamicin damages sensory hair cells in the inner ear, leading to hearing loss. The mechanism involves toxic effects on cochlear cells. Inflammation can exacerbate gentamicin's ototoxicity.
Gentamicin enters hair cells more easily during inflammation via the TRPV1 protein. Lack of functional TRPV1 can protect against gentamicin-induced hearing loss.
Our understanding of gentamicin's impact on the inner ear continues to evolve as research sheds light on the intricate processes involved.
What Is the Mechanism of Action of Gentamicin Ear Drops?
Gentamicin ear drops operate by infiltrating the ear canal to combat inner ear infections. This entails gentamicin binding to bacterial ribosomes, hindering protein synthesis, and impeding bacterial growth.
Effective against several gram-negative and some gram-positive bacteria, these drops are targeted and spare the patient systemic side effects common in oral or injectable antibiotics.
Typically prescribed for otitis externa or middle ear infections, gentamicin ear drops deliver precise treatment directly to the affected area.
Conclusion
In conclusion, understanding the ototoxic mechanisms of gentamicin is crucial in preventing irreversible damage to hearing function.
By identifying risk factors, monitoring for hearing loss, and implementing strategies to minimize its impact, healthcare providers can ensure safer use of gentamicin in practice.
Like a diligent watchman guarding a precious treasure, vigilant monitoring and timely interventions can protect the delicate cochlear hair cells from the destructive effects of gentamicin-induced ototoxicity.