Understanding Hearing Loss
Which of the Following Is Not a Cause of Conductive Hearing Loss?
Not all factors contribute to conductive hearing loss – discover which surprising cause doesn't align with this type of auditory impairment.

It’s interesting to observe that around 90% of hearing loss instances are identified as either conductive or mixed hearing loss when delving into the reasons behind conductive hearing loss.
Now, when pondering the question of which of the following is not a cause of conductive hearing loss, one might be surprised to learn that not all factors contribute to this type of hearing impairment.
Let's explore the intricacies of the outer and middle ear issues that typically lead to conductive hearing loss and uncover why one of the options provided does not align with this particular type of auditory deficiency.
Key Takeaways
- Presbycusis (Age-Related Hearing Loss) is not a cause of Conductive Hearing Loss.
- Otosclerosis, Noise-Induced Hearing Loss, and Meniere's Disease are potential causes.
- Conductive Hearing Loss is primarily due to issues in the ear canal or middle ear.
- Understanding distinct causes helps in accurate diagnosis and appropriate treatment.
Earwax Impaction
Earwax impaction occurs when excessive buildup of earwax obstructs the ear canal, causing conductive hearing loss. This blockage interferes with the transmission of sound waves to the eardrum, leading to symptoms like earache, tinnitus, and decreased hearing. To address earwax impaction, treatment options include using ear drops to soften the wax, irrigation to flush it out, or manual removal by a healthcare provider. When earwax accumulates and hardens in the ear canal, it can significantly impact one's ability to hear clearly, highlighting the importance of prompt intervention.
Manual removal by a healthcare professional is often necessary for severe cases of earwax impaction to ensure the safe and effective clearance of the ear canal. It's crucial to address earwax impaction promptly to prevent potential hearing issues and discomfort. Regular ear hygiene practices, such as using ear drops to soften wax and gently cleaning the ears, can help prevent the buildup of earwax and reduce the risk of developing conductive hearing loss.
Presbycusis
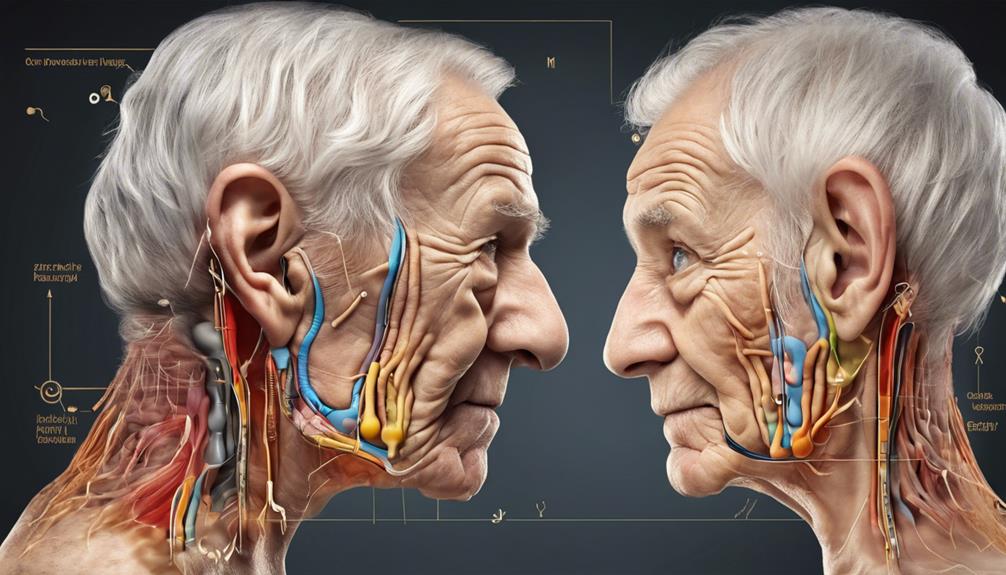
Presbycusis, also known as age-related hearing loss, is a condition that predominantly affects the inner ear and is distinct from conductive hearing loss primarily associated with outer or middle ear issues.
- Presbycusis is an age-related condition leading to sensorineural hearing loss.
- It affects the cochlea, an essential structure in the inner ear responsible for hearing.
- The auditory nerve, which transmits sound signals to the brain, is also impacted by presbycusis.
- Unlike conductive hearing loss, which involves issues like cerumen impaction or otitis media, presbycusis results from degeneration within the inner ear.
Understanding the differences between presbycusis and conductive hearing loss is crucial for accurate diagnosis and treatment planning. As individuals age, the likelihood of experiencing presbycusis increases, making it essential to recognize the unique characteristics of this age-related hearing impairment. By focusing on the inner ear mechanisms affected by presbycusis, healthcare professionals can provide targeted interventions to help individuals manage this form of hearing loss effectively.
Otosclerosis
Abnormal bone growth in the middle ear characterizes otosclerosis, a condition that commonly leads to conductive hearing loss. Otosclerosis specifically affects the stapes bone, one of the tiny bones in the middle ear responsible for transmitting sound vibrations to the inner ear. This abnormal bone growth causes the stapes bone to become fixed, reducing its ability to conduct sound effectively. As a result, individuals with otosclerosis may experience hearing difficulties, especially in the lower frequencies.
To address otosclerosis and restore hearing function, surgical intervention is often necessary. A procedure called stapedectomy involves removing a portion of the stapes bone and replacing it with a prosthesis to improve sound transmission. This surgery can significantly improve hearing outcomes for individuals with otosclerosis, offering them a chance to regain quality of life through enhanced auditory function.
| Key Points | Details |
|---|---|
| Condition | Abnormal bone growth in the middle ear |
| Affected Bone | Stapes bone |
| Treatment | Surgical intervention, specifically stapedectomy |
Noise-Induced Hearing Loss

Noise exposure can have detrimental effects on our hearing, particularly causing damage to the inner ear sensory cells and leading to noise-induced hearing loss. When loud sounds impact the ear over time, the delicate hair cells within the cochlea can become damaged, resulting in sensorineural hearing loss.
To prevent noise-induced hearing loss, individuals can use ear protection in environments where loud sounds are prevalent. Unlike conductive hearing loss, which often involves issues in the outer or middle ear, noise-induced hearing loss specifically targets the inner ear sensory cells.
Understanding the distinctions between conductive and sensorineural hearing loss is crucial for accurately diagnosing and treating these conditions. By recognizing the impact of noise exposure on our hearing and taking proactive measures to protect our ears, we can mitigate the risk of developing this type of hearing impairment.
Meniere's Disease
Meniere's Disease, a disorder affecting the inner ear's balance and hearing functions, presents symptoms such as vertigo, hearing loss, tinnitus, and a sensation of fullness in the ear. This condition is characterized by episodes of vertigo, a spinning sensation that can be debilitating. The exact cause of Meniere's disease isn't fully understood, but it's believed to be associated with fluid buildup in the inner ear. The increased fluid pressure affects the function of the inner ear, leading to the symptoms experienced by individuals with this condition.
In addition to vertigo, individuals with Meniere's disease may also experience fluctuating hearing loss, typically in one ear. Tinnitus, a ringing or buzzing sound in the ear, is another common symptom. The feeling of fullness in the ear is often described as similar to having pressure or blockage in the ear canal.
Treatment for Meniere's disease aims to manage symptoms and may include dietary modifications, medication to reduce fluid retention, and in severe cases, surgical interventions to alleviate pressure in the inner ear.
Frequently Asked Questions
What Are the Causes of Conductive Hearing Loss?
We'll cover the various causes of conductive hearing loss, which primarily stem from issues in the outer or middle ear. Common culprits include cerumen impaction, otitis media, and otosclerosis. Factors like foreign objects, perforated eardrums, and middle ear infections also contribute to this type of hearing loss.
Which of the Following Would Cause Conductive Hearing Loss?
We'll start by exploring the factors that contribute to conductive hearing loss.
Accumulated cerumen, damaged hair cells, middle ear infections, inflamed tympanic membrane, and otosclerosis are all known culprits. Each of these conditions can impede sound transmission through the ear, leading to hearing difficulties.
Understanding these causes is crucial for diagnosing and treating conductive hearing loss effectively.
Which of the Following Is Not a Possible Cause of Conduction?
When considering causes of conductive hearing loss, it's essential to rule out cochlear nerve degeneration. This condition isn't a factor in conductive hearing loss, which typically stems from problems in the outer or middle ear.
Factors like impacted cerumen, otitis media, and otosclerosis are common culprits. Conductive hearing loss interferes with sound wave transmission.
Notably, presbycusis, age-related hearing loss, doesn't contribute to conductive hearing loss.
Is Otitis Media a Cause of Conductive Hearing Loss?
Yes, otitis media can cause conductive hearing loss. The fluid buildup and inflammation associated with this condition can disrupt sound conduction and affect the movement of auditory ossicles.
It's a common cause of conductive hearing loss, particularly in children. Prompt treatment is crucial to prevent long-term hearing issues.
It's essential to address otitis media promptly to avoid potential complications with hearing.
Conclusion
In conclusion, it's important to note that presbycusis isn't a cause of conductive hearing loss. This age-related hearing loss is actually classified as sensorineural deafness, not conductive.
When it comes to conductive hearing loss, causes such as earwax impaction, otosclerosis, noise-induced hearing loss, and Meniere's disease are more commonly associated.
To exaggerate slightly, understanding the distinction between these different types of hearing loss is as crucial as hearing a pin drop in a thunderstorm.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Windows High Volume Can Cause Hearing Loss: Tips to Protect Your Ears
Wander into the world of windows high volume and learn how it silently impacts your hearing health – the secrets to safeguarding your ears await!

Let’s be honest, the allure of blasting music through the windows is undeniable, but have you ever thought about the potential effects on our auditory health?
As we navigate through our daily lives, the constant exposure to loud noises can quietly take a toll on our ears without us even realizing it.
Understanding how this seemingly harmless habit can lead to potential hearing loss is crucial.
Stay tuned as we unravel the secrets of protecting our ears and discover practical tips to safeguard our auditory well-being in a world filled with noise.
Key Takeaways
- High volume from windows can damage hearing by harming delicate ear cells.
- Protect ears with earplugs or breaks to prevent irreversible auditory damage.
- Regular check-ups detect and prevent worsening hearing loss from high volumes.
- Be mindful of noise levels to avoid immediate and long-term hearing issues.
Understanding the Impact of High Volume
Exposure to high volume sounds can have detrimental effects on our hearing health, causing damage to the delicate hair cells in the ear and potentially leading to permanent hearing loss. Volume can cause Hearing.
The impact of high volume on hearing is profound and often underestimated. Prolonged exposure to loud noise, whether from music, machinery, or other sources, can result in irreversible damage to the auditory system. This damage primarily affects the hair cells in the cochlea, which are responsible for translating sound vibrations into electrical signals that the brain can interpret. When these hair cells are subjected to high volumes, they can become overworked and eventually die off, leading to hearing loss.
Additionally, exposure to loud noise can also trigger the development of tinnitus, a condition characterized by persistent ringing or buzzing in the ears. It's crucial to understand that even short bursts of high volume sounds, such as explosions or gunshots, can cause immediate and severe damage to our hearing.
Therefore, taking proactive measures to protect our ears from excessive noise exposure is essential for preserving our hearing health in the long term.
Common Symptoms of Hearing Damage
Indications of hearing damage commonly include persistent ringing in the ears, difficulty in understanding speech clearly, and a sense of sounds being muffled. Individuals with hearing damage may also exhibit sensitivity to loud noises and find it challenging to follow conversations in noisy environments. As part of ear protection, recognizing these symptoms early is crucial to prevent further damage and maintain overall hearing health. Below is a table summarizing common symptoms of hearing damage:
| Symptom | Description |
|---|---|
| Ringing in the ears (tinnitus) | Persistent noise or ringing sensation in one or both ears. |
| Difficulty understanding speech | Struggle to comprehend conversations, especially in noisy or crowded settings. |
| Muffled sounds | Sensation of sounds being unclear, dulled, or lacking sharpness. |
Being attentive to these signs and seeking professional evaluation promptly can aid in the management and prevention of hearing loss. Remember, early intervention plays a key role in protecting your ears and preserving your hearing abilities.
Risks of Prolonged Exposure
Continuously exposing oneself to high volume levels poses a significant risk to the delicate hair cells in the inner ear, potentially leading to irreversible damage and long-term hearing issues. High volume can cause various detrimental effects on hearing health, including:
- Development of Tinnitus: Prolonged exposure to high volume levels can result in the development of tinnitus, a condition characterized by a persistent ringing, buzzing, or hissing sound in the ears. This debilitating condition can significantly impact quality of life and may be challenging to manage.
- Noise-Induced Hearing Loss: High volume exposure is a common cause of noise-induced hearing loss, particularly in industries with high noise levels. This type of hearing loss is often gradual but can lead to permanent damage if preventive measures aren't taken.
- Immediate Auditory Damage: Even brief exposures to loud noise can cause immediate damage to the auditory system. This underscores the importance of protecting your ears from high volume levels to prevent both short-term and long-term consequences.
Effective Ways to Protect Your Ears

To safeguard our hearing health, implementing effective strategies to protect our ears is paramount in preventing potential damage from high volume exposure. Wearing earplugs or earmuffs in noisy environments significantly reduces the risk of hearing loss by acting as a barrier against loud sounds.
Taking regular breaks from prolonged exposure to loud noises allows your ears to recover and lowers the chances of overexposure. It's crucial to maintain safe volume levels when using headphones to prevent hearing damage. Opting for noise-canceling headphones can help reduce external noise, allowing you to listen at lower volumes without compromising sound quality.
Additionally, being mindful of noise levels in recreational activities like concerts can safeguard your ears from potential harm. By incorporating these practices into our daily routines, we can proactively protect our hearing and reduce the risk of hearing loss associated with high volume environments.
Importance of Regular Hearing Check-Ups
Regular monitoring of one's hearing health through routine check-ups is crucial for early detection and prevention of potential hearing loss. Here are three key reasons why regular hearing check-ups are essential:
- Early Detection: Regular check-ups can help identify early signs of hearing loss that may otherwise go unnoticed. Detecting hearing impairment in its initial stages allows for timely intervention and management strategies to be implemented.
- Assessment of Hearing Impairment: Hearing screenings conducted during check-ups can assess the extent of any existing hearing impairment. These assessments provide valuable information about the level of hearing loss and guide professionals in developing personalized treatment plans.
- Prevention of Deterioration: Early intervention through regular check-ups can prevent further deterioration of hearing. Monitoring changes in hearing health over time enables healthcare providers to intervene proactively and implement measures to preserve and protect the individual's hearing capabilities. Regular check-ups are, therefore, crucial for maintaining optimal ear health and overall well-being.
Frequently Asked Questions
Can Driving With the Windows Down Damage Your Hearing?
Yes, driving with the windows down can damage our hearing. Noise levels inside a car at highway speeds can exceed safe limits, leading to potential hearing loss over time.
It's essential to be cautious of this risk and take steps to protect our ears from prolonged exposure to loud wind noise while driving. Using ear protection like earplugs or noise-canceling headphones can help mitigate this danger and safeguard our hearing health.
How Do I Turn off Ear Protection in Windows?
Sure thing!
To turn off ear protection in Windows, right-click on the volume icon. Choose 'Sounds' then 'Playback' to find device settings. Double click on the playback device and uncheck the ear protection option. Apply the changes and test volume adjustments.
This simple process can help prevent sudden loud volume spikes that may cause hearing loss. Remember, always prioritize your ear health by taking such precautions.
How Can I Protect My Ears From Hearing Loss?
We can safeguard our hearing by using ear protection in loud environments, taking breaks from loud sounds, and maintaining safe volume levels with headphones.
Noise-canceling headphones can reduce the need for high volumes. Being aware of noise levels in activities like concerts is crucial for hearing health.
Regularly implementing these practices helps prevent damage to delicate ear structures and minimizes the risk of hearing loss.
How Can You Protect Yourself From Excessive Sound?
To protect ourselves from excessive sound, we must be vigilant about our surroundings and exposure to loud noises. Utilizing ear protection like earplugs or earmuffs, taking breaks from noisy environments, and maintaining safe volume levels with headphones are essential strategies. Noise-canceling headphones can also help reduce external noise, minimizing the need for high volumes.
Being mindful in recreational settings, like concerts, can prevent sudden exposure to damaging sound levels.
Conclusion
In conclusion, we must recognize the importance of protecting our ears from high volume to prevent hearing loss. By taking proactive measures such as using earplugs and maintaining safe volume levels, we can safeguard our hearing health.
Regular hearing check-ups are crucial to monitor any potential damage. Let's remember that our ears are delicate and valuable, and by prioritizing their protection, we can enjoy a lifetime of clear and healthy hearing.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Nasal Congestion Can Cause Hearing Loss: A Guide
Navigate the link between nasal congestion and hearing loss to uncover surprising connections that may affect your health in unexpected ways.
Ever thought about the effect of nasal congestion on your ability to hear? Grasping the complex link between these apparently unconnected problems can illuminate potential issues that are often ignored.
As we explore the subtle yet significant ways nasal congestion can lead to hearing loss, you'll discover practical insights that could make a difference in your overall well-being.
Key Takeaways
- Nasal congestion disrupts Eustachian tube function, affecting pressure balance in the ear.
- Congestion can lead to fluid buildup, hindering sound transmission and causing ear fullness.
- Prompt management of congestion is crucial to prevent complications and preserve hearing health.
- Consulting an ENT specialist helps diagnose and treat congestion-related hearing issues effectively.
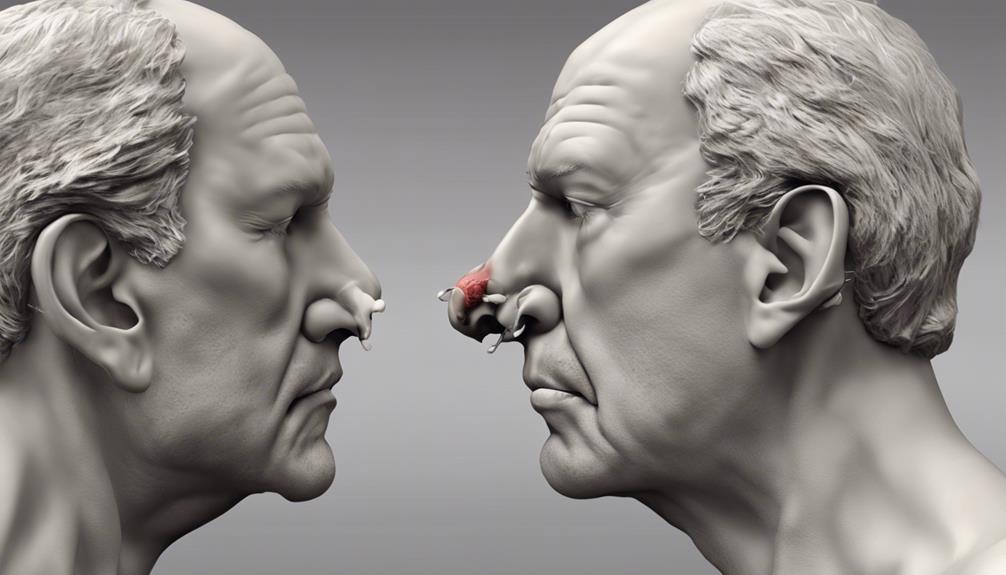
The Link Between Nasal Congestion and Hearing
Experiencing nasal congestion can directly impact our hearing by causing blockages in the Eustachian tube, disrupting the pressure balance within the ear. The Eustachian tube plays a crucial role in regulating the pressure in the middle ear. When this tube gets blocked due to nasal congestion, it can lead to difficulties in equalizing pressure, resulting in a feeling of fullness in the ears and potential fluid buildup. This fluid accumulation can interfere with the proper functioning of the inner ear, affecting sound transmission and leading to temporary hearing loss.
Sinus infections and persistent nasal congestion can exacerbate these issues, making it essential to address nasal congestion promptly to prevent further complications with hearing. Consulting an ENT specialist can help diagnose the root cause of the congestion and provide appropriate treatment to alleviate the symptoms and improve overall hearing health. By addressing nasal congestion effectively, individuals can mitigate the impact on their hearing and enhance their quality of life.
Impact of Congestion on Hearing Function
When nasal congestion impedes the Eustachian tube, it can directly impact the function of hearing by disrupting the pressure equilibrium in the ear. The blockage of the Eustachian tube hinders the equalization of pressure in the middle ear, leading to hearing loss as sound waves struggle to reach the inner ear. Additionally, the increased mucus production resulting from congestion can cause a sense of fullness in the ears and reduce the ability to hear clearly. Pressure buildup in the sinuses due to congestion can further contribute to a feeling of muffled or distorted hearing. Fortunately, congestion-related hearing loss is typically temporary and can be alleviated by addressing the underlying sinus issues. To emphasize the effects of congestion on hearing function, consider the following table:
| Issue | Impact on Hearing |
|---|---|
| Eustachian tube blockage | Disrupted pressure equilibrium |
| Increased mucus production | Feeling of ear fullness, reduced clarity |
| Sinus pressure buildup | Muffled or distorted hearing |
Understanding Nasal Issues and Hearing Loss
Understanding the intricate connection between nasal issues and hearing loss is crucial for effectively managing potential impacts on one's auditory health. Nasal congestion can lead to hearing loss due to its direct influence on the Eustachian tubes, responsible for equalizing pressure in the ears. Inflammation and swelling caused by conditions like sinusitis can affect these tubes, leading to mucus buildup and blockages that disrupt normal hearing function. Individuals experiencing nasal congestion may notice symptoms such as ear pressure, muffled sounds, and challenges in equalizing ear pressure.
To address these issues and preserve hearing care, it's essential to promptly manage nasal congestion. Home remedies like steam inhalation can help alleviate congestion, reducing the risk of hearing loss associated with Eustachian tube dysfunction. By taking proactive steps to relieve nasal issues, individuals can mitigate the potential impact on their hearing health and maintain optimal auditory function.
Remedies for Nasal Congestion-Related Hearing Problems

When dealing with nasal congestion-related hearing problems, relief can be found through various effective remedies. Here are three key strategies to help alleviate the impact of nasal congestion on your hearing:
- Use Nasal Sprays: Opt for saline nasal sprays to clear out mucus and allergens from your nasal passages, allowing for improved airflow and reduced pressure on the Eustachian tube. This can aid in restoring normal hearing function.
- Stay Hydrated: Keeping yourself well-hydrated can help thin out mucus in your sinuses and nasal passages, making it easier to drain and reducing the chances of sinusitis or middle ear infections that could affect your hearing.
- Steam Inhalation: Inhaling steam with hot water or essential oils can provide quick relief for a stuffy nose, opening up the Eustachian tube and alleviating ear pressure. This natural remedy can contribute to improved hearing clarity by reducing congestion.
Preventing Hearing Loss Due to Nasal Congestion
To prevent potential hearing loss resulting from nasal congestion, it's essential to address the underlying causes promptly and effectively. When nasal congestion leads to Eustachian tube blockage, it can disrupt pressure regulation in the middle ear, causing issues with hearing.
The buildup of mucus from nasal congestion can further impact the transmission of sound to the inner ear, resulting in muffled hearing. Sinus pressure due to nasal congestion can also lead to ear discomfort and affect the ability to hear clearly.
Drinking plenty of fluids can help thin mucus and alleviate congestion, potentially preventing hearing loss. Seeking guidance from an Ear, Nose, and Throat (ENT) specialist is advisable for persistent nasal congestion-related hearing problems.
In cases where allergic reactions or a runny nose are persistent and causing hearing difficulties, professional evaluation is crucial to prevent long-term complications like sensorineural hearing loss.
Frequently Asked Questions
Can Nasal Congestion Cause Loss of Hearing?
Yes, nasal congestion can cause loss of hearing. When congestion blocks the Eustachian tube, which regulates middle ear pressure, it can impact sound transmission and result in muffled hearing.
Increased mucus production from congestion can also lead to ear pressure and fluid buildup in the middle ear, affecting hearing function.
Addressing nasal congestion promptly is crucial to prevent potential hearing issues associated with Eustachian tube blockage.
How Do You Get Rid of Hearing Loss From a Cold?
When faced with hearing loss from a cold, we can take steps to alleviate the symptoms. Remedies such as nasal decongestants, steam inhalation, and warm compresses can help clear congestion and restore hearing.
It's essential to address any middle ear infections promptly as they can contribute to temporary hearing loss during a cold. Seeking professional evaluation if the hearing loss persists is crucial to rule out any underlying issues.
How Does Congestion Clog Ears?
When congestion strikes, it's like a traffic jam in our ears. The Eustachian tube, responsible for regulating ear pressure, can get blocked by mucus buildup.
This blockage causes a feeling of fullness and can even muffle sounds. The pressure changes in the ear due to excess mucus can distort sound transmission, affecting our hearing clarity.
It's crucial to address congestion to keep our ears in top shape.
Can Sudden Hearing Loss Be Restored?
Yes, sudden hearing loss can sometimes be restored. Prompt medical attention is crucial to maximize the chances of recovery.
Treatment options like corticosteroids, antiviral medications, and hyperbaric oxygen therapy may help. The success rate varies, with some achieving full restoration and others facing permanent damage.
The underlying cause, such as viral infections or vascular issues, plays a significant role in the prognosis. Immediate evaluation by an ear, nose, and throat specialist is essential for determining the best course of action.
Conclusion
Just as a tangled knot can hinder our progress, nasal congestion can obstruct our ability to hear clearly. By unraveling the issues causing congestion, we can untangle the barriers to optimal hearing health.
Let's navigate the twists and turns of our nasal passages with care, seeking clarity and relief. Remember, addressing the root of the problem can lead us down a path of improved hearing and well-being.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Heart Problems Can Cause Hearing Loss: A Comprehensive Guide
Prepare to be amazed by the unexpected link between heart issues and hearing loss – the surprising connection will leave you eager for more!
Truth be told, we frequently overlook how interconnected our bodily systems are when it comes to our health.
However, have you ever pondered how issues with the heart could potentially impact something as seemingly unrelated as our hearing?
The intricate relationship between cardiovascular health and hearing function might surprise you.
In this guide, we explore the subtle yet profound ways heart problems can lead to changes in our auditory abilities.
Stay tuned to uncover the intricate details of this fascinating connection that could reshape your perspective on overall well-being.
Key Takeaways
- Cardiovascular issues impact blood flow to the inner ear, affecting hearing sensitivity.
- Plaque buildup in arteries can harm inner ear nerves, leading to hearing loss.
- Hearing changes may serve as an early warning sign of underlying heart conditions.
- Managing cardiovascular health is crucial in preserving auditory function and preventing heart-related hearing loss.
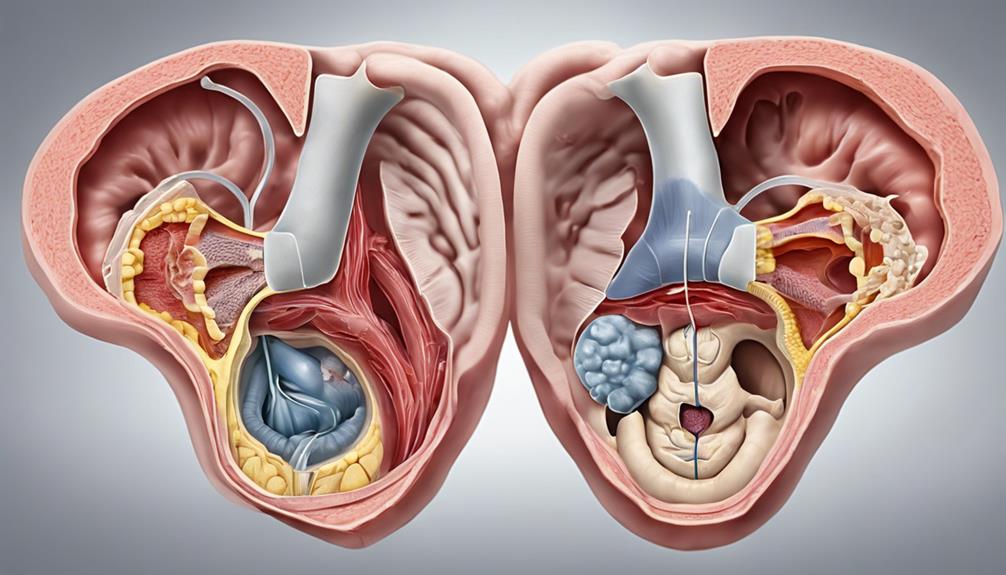
Mechanisms of Heart-Related Hearing Loss
Plaque buildup in arteries stemming from heart disease can harm the inner ear nerves sensitive to blood flow, potentially resulting in hearing loss. This process, known as sensorineural hearing loss, is mainly characterized by a decreased ability to hear low-frequency sounds. When cardiovascular risk factors lead to reduced blood flow to the inner ear, the auditory function is compromised, impacting the transmission of sound signals to the brain.
The intricate connection between cardiovascular health and hearing underscores the importance of maintaining a healthy heart to preserve optimal auditory function. The inner ear's vulnerability to cardiovascular issues highlights how heart disease can have direct implications on hearing abilities. By understanding the mechanisms behind heart-related hearing loss, individuals can recognize that changes in their hearing may signal underlying cardiovascular problems, emphasizing the interplay between heart health and auditory well-being.
This insight positions heart-related hearing loss as a potential early warning sign for broader cardiovascular issues, emphasizing the significance of holistic health management.
Warning Signs of Hearing Impairment
A common indication of potential hearing impairment is experiencing difficulty understanding speech, often leading individuals to frequently ask others to repeat themselves. This difficulty can be exacerbated in noisy environments, where background noise can make it challenging to discern words clearly.
Warning signs of hearing impairment associated with heart conditions may also manifest in various ways:
- Tinnitus: The presence of a ringing or buzzing sound in the ears can be a warning sign of underlying hearing issues related to cardiovascular problems.
- Ear Pain: Discomfort or pain in the ears may indicate a need for further evaluation of potential hearing loss linked to heart conditions.
- Dizziness and Imbalance: Feeling unsteady or experiencing frequent bouts of dizziness can be symptomatic of hearing impairment associated with cardiovascular issues.
- Changes in Frequency Perception: Difficulty hearing high or low-frequency sounds could be a signal of potential hearing loss related to heart problems, warranting prompt attention and assessment.
Cardiovascular Health and Auditory System
Reduced blood flow to the inner ear due to cardiovascular issues can have a significant impact on sensorineural hearing loss, linking cardiovascular health intricately with the auditory system. Conditions such as hypertension and coronary artery disease are often associated with worsened low-frequency hearing due to their effects on the blood supply to the inner ear.
Atherosclerosis, characterized by plaque buildup in arteries, can strain the heart and further diminish the circulation of blood to the delicate structures involved in hearing. This impaired cardiovascular health doesn't just affect the peripheral auditory system but can also have repercussions on the central auditory system, impacting how sound signals are processed in the brain.
Implementing lifestyle changes to improve cardiovascular health, such as managing hypertension and overall heart health, is crucial in potentially mitigating the risk of hearing loss associated with these conditions. By prioritizing cardiovascular well-being, individuals may also be safeguarding their auditory function against the detrimental effects of cardiovascular diseases.
Protecting Your Hearing Health
To safeguard your hearing health, incorporating regular cardiovascular exercise into your routine can play a crucial role in improving blood flow to the inner ear and protecting against potential hearing loss. Here are four key actions to consider for maintaining optimal hearing health:
- Maintain a Balanced Diet: Consuming heart-healthy foods rich in nutrients like omega-3 fatty acids and antioxidants can benefit both your cardiovascular system and your hearing health.
- Manage Blood Pressure: Keeping your blood pressure within a healthy range reduces the risk of damage to the blood vessels in the inner ear, promoting better hearing outcomes.
- Schedule Regular Hearing Screenings: Including hearing evaluations in your routine medical check-ups can aid in the early detection of any hearing issues related to heart conditions, allowing for timely intervention.
- Seek Collaborative Care: Coordinating care between cardiovascular specialists and audiologists can lead to comprehensive management strategies that address both heart and hearing health needs effectively.
Understanding the Heart-Hearing Connection
Exploring the intricate relationship between cardiovascular health and hearing function reveals significant insights into the interconnected nature of the heart and auditory systems. Cardiovascular diseases can result in reduced blood flow to the inner ear, potentially leading to hearing loss. Plaque buildup in arteries, a consequence of conditions like atherosclerosis, can damage nerves within the inner ear, thus affecting hearing abilities.
Interestingly, studies suggest that hearing loss may act as an early indicator of heart disease, underscoring the strong link between the two systems. The inner ear is particularly sensitive to blood flow, making it vulnerable to damage from cardiovascular issues. This sensitivity emphasizes the critical role of heart health in preserving hearing.
Notably, experts such as Dr. David R. Friedland emphasize the positive impact of good cardiovascular health on hearing outcomes, highlighting the importance of adopting preventive measures to support both heart and hearing health. By understanding this intricate connection, individuals can take proactive steps to safeguard their cardiovascular and auditory well-being.
Frequently Asked Questions
How Does Heart Disease Cause Hearing Loss?
Heart disease can lead to hearing loss by impacting blood flow to the inner ear, causing damage to the delicate structures responsible for hearing.
Plaque buildup in arteries can restrict blood flow, affecting auditory function. Cardiovascular issues can reduce blood supply to the cochlea, resulting in sensorineural hearing loss.
Inner ear nerves are sensitive to changes in blood flow, making them vulnerable to damage from heart problems.
What Are the 4 Signs Your Heart Is Quietly Failing?
We've learned that four subtle signs of quietly failing hearts include shortness of breath, fatigue, leg swelling, and persistent coughing. These symptoms may hint at underlying heart problems that need attention.
Monitoring changes in heart rate, blood pressure, and energy levels is crucial for early detection. Regular medical check-ups and cardiovascular assessments can help catch silent heart failure.
Recognizing sudden weight gain, reduced exercise tolerance, and increased heart rate can also signal heart issues.
What Are the Early Signs of Heart Blockage?
We can recognize early signs of heart blockage by being vigilant for symptoms such as:
- Chest pain
- Shortness of breath
- Fatigue during physical activity
- Dizziness
- Lightheadedness
- Fainting spells
- Irregular heartbeats
- Palpitations
Swelling in the legs, ankles, or feet can also indicate compromised circulation. Regular monitoring of blood pressure and cholesterol levels, along with prompt medical evaluation, can help detect and address these warning signs before they escalate.
Can a Blocked Artery Cause Hearing Loss?
Yes, a blocked artery can cause hearing loss. When blood flow to the inner ear is restricted, the delicate hair cells in the cochlea can be damaged, leading to impairment.
Plaque buildup in arteries, such as from atherosclerosis, can hinder inner ear function. The sensitivity of inner ear nerves to changes in blood flow makes them susceptible to cardiovascular issues.
Early detection of hearing loss can serve as a warning sign for potential heart problems.
Conclusion
In conclusion, the intricate relationship between heart problems and hearing loss highlights the importance of maintaining cardiovascular health for optimal auditory function.
By recognizing the warning signs of hearing impairment and taking proactive steps to protect our hearing, we can work towards preventing potential complications.
Understanding the mechanisms behind heart-related hearing loss empowers us to make informed decisions for our overall well-being.
Stay tuned for more insights on how to safeguard your heart and hearing health!
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
-
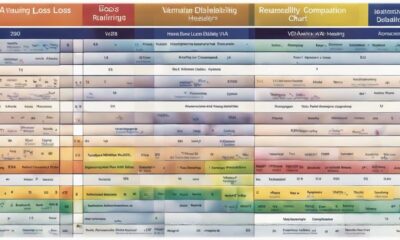
 Navigating the VA System1 month ago
Navigating the VA System1 month agoVA Hearing Loss Rating Chart: Understanding Disability Compensation
-

 Therapies and Interventions2 weeks ago
Therapies and Interventions2 weeks ago10 Auditory Processing Goals for Effective Speech Therapy
-

 Vetted2 months ago
Vetted2 months ago15 Best Oticon Hearing Aids to Improve Your Hearing in 2024
-

 Tinnitus2 months ago
Tinnitus2 months agoVA's Rating System for Tinnitus and Hearing Loss Explained
-

 Navigating the VA System1 month ago
Navigating the VA System1 month agoUnderstanding Bilateral Hearing Loss VA Rating Criteria
-

 Sign Language2 weeks ago
Sign Language2 weeks agoMastering the Art of Signing Letters in Sign Language
-

 Sign Language2 weeks ago
Sign Language2 weeks agoSign Language Emoji Translator: How to Communicate With Gestures
-

 Sign Language3 months ago
Sign Language3 months agoMedical Sign Language PDF: A Comprehensive How-To Guide


















