Exploring the intricate connection between Osteogenesis Imperfecta (OI) and hearing loss is like trying to find your way through a hidden path in a dense forest, where each discovery sheds light on the next mystery.
The link between these two seemingly disparate conditions intrigues us, making us question the underlying mechanisms at play.
As we delve into the complexities of OI's impact on auditory function, we begin to unravel a fascinating web of genetic mutations, bone structures, and collagen deficiencies that contribute to this phenomenon.
Join us on this journey as we unravel the enigmatic bond between OI and hearing loss.
Key Takeaways
- Mutations in collagen genes disrupt inner ear structures.
- Abnormal bone affects sound transmission pathways.
- Collagen deficiencies lead to diverse types of hearing loss.
- Vulnerable inner ear components contribute to hearing impairment.
Genetic Mutation and Hearing Loss
Genetic mutations in the COL1A1 and COL1A2 genes, impacting the synthesis of type I collagen, are significant contributors to the development of hearing loss in individuals with Osteogenesis Imperfecta (OI). The prevalence of hearing loss in OI patients ranges from 46% to 72%, with sensorineural hearing loss more prevalent in older individuals and conductive hearing loss more common in younger patients. This variation in hearing loss severity, ranging from mild to profound, poses challenges in diagnosis and treatment.
Sensorineural hearing loss in OI patients is often linked to complications such as cochlear atrophy and abnormal bone formation. Unlike otosclerosis, sensorineural hearing loss in OI is more prevalent due to these factors. The nature of genetic mutations in COL1A1 and COL1A2 genes doesn't directly correlate with the type of hearing loss experienced by OI patients.
Treatment options for hearing loss in OI include hearing aids, stapes surgery, and cochlear implants, although management can be complex due to associated tympanometric abnormalities and middle ear pathologies.
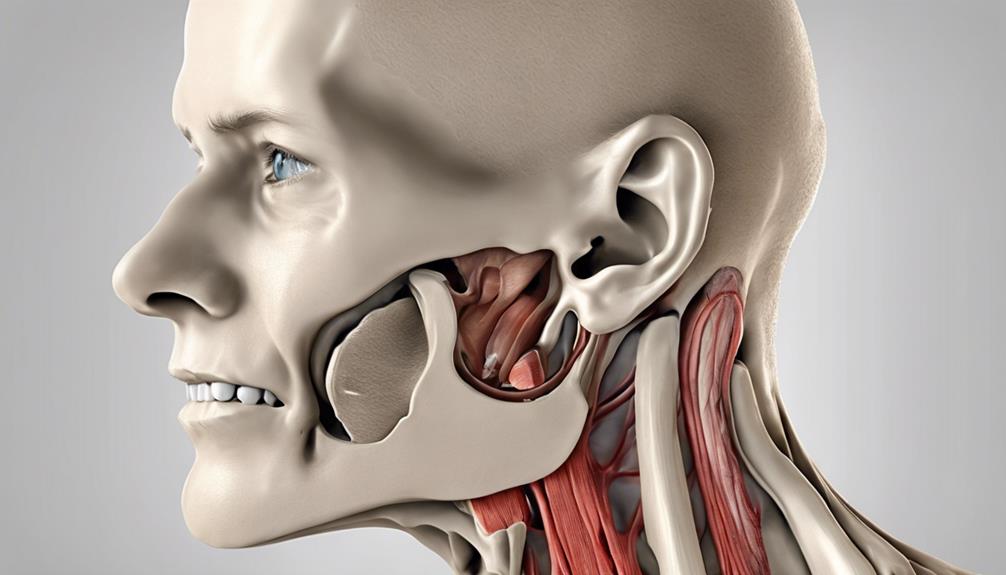
Bone Structure Impact on Auditory System

The impact of abnormal bone structure in Osteogenesis Imperfecta extends to the auditory system, affecting the transmission of sound waves and structures vital for hearing function. In OI, the structural abnormalities can lead to both conductive and sensorineural hearing loss. Conductive hearing loss occurs when the transmission of sound waves is disrupted due to abnormal bony formation, affecting the ossicles responsible for sound conduction. On the other hand, sensorineural hearing loss is linked to changes in type I collagen synthesis, impacting inner ear structures like the cochlea and auditory nerve. These alterations in OI can influence the cochlea and other inner ear structures, contributing to various types of hearing loss. The table below summarizes the impact of bone structure abnormalities in OI on the auditory system:
| Hearing Loss Type | Description | Examples |
|---|---|---|
| Conductive Hearing Loss | Results from issues in the outer or middle ear that block sound conduction. | Ossicle malformations |
| Sensorineural Hearing Loss | Caused by damage to the inner ear or auditory nerve, affecting sound processing. | Cochlear abnormalities |
Understanding the connection between bone structure and the auditory system in OI is crucial for managing and addressing the associated hearing impairments effectively.
Collagen Deficiency and Auditory Function
Our investigation into collagen deficiency and its impact on auditory function reveals crucial insights into the mechanisms underlying hearing loss in Osteogenesis Imperfecta.
In OI, mutations affecting the synthesis of type I collagen have profound implications for the auditory system. Type I collagen deficiencies impact the integrity of inner ear structures, including the ossicles and cochlear structures, essential for sound transmission and processing.
These changes contribute to auditory dysfunction in OI patients, manifesting as conductive hearing loss due to abnormalities in bone conduction pathways. Additionally, sensorineural changes resulting from collagen abnormalities also play a significant role in the auditory impairments observed in individuals with OI.
The varied types of hearing loss experienced by OI patients, such as conductive, sensorineural, or mixed, highlight the complex interactions between collagen abnormalities and the delicate structures of the auditory system. Understanding the intricate relationship between collagen deficiency and auditory function is essential for addressing the diverse manifestations of hearing loss in OI.
Inner Ear Vulnerability in OI
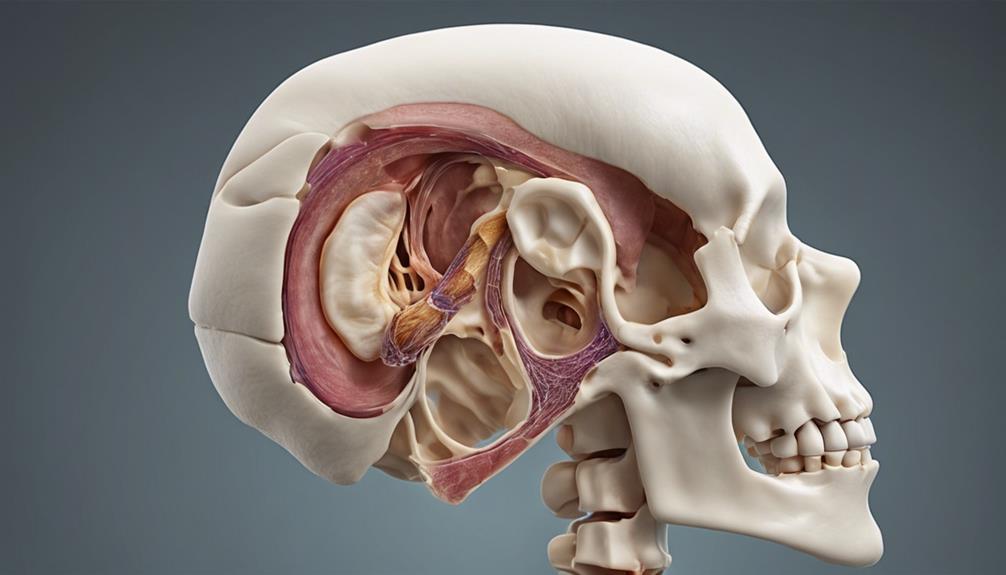
Examining the inner ear vulnerability associated with Osteogenesis Imperfecta reveals critical insights into the mechanisms underlying hearing loss in affected individuals. The ossicles and cochlea in OI patients are particularly vulnerable, leading to both conductive and sensorineural hearing loss. Changes in type I collagen synthesis, crucial for maintaining the integrity of inner ear components, significantly impact auditory function. Inner ear abnormalities in OI can manifest in various ways, causing conductive, sensorineural, or mixed patterns of hearing loss. Structural defects linked to the pathophysiology of OI compromise the auditory pathways, resulting in diverse types of hearing impairment.
| Inner Ear Vulnerability in OI | Effects | Implications |
|---|---|---|
| Vulnerability of ossicles and cochlea | Conductive and sensorineural hearing loss | Altered auditory function |
| Changes in type I collagen synthesis | Integrity of inner ear components | Impacted auditory function |
| Inner ear abnormalities in OI | Mixed hearing loss patterns | Varied effects on auditory pathways |
| Structural defects in OI pathophysiology | Compromised auditory pathways | Diverse types of hearing impairment |
Treatment Approaches for Hearing Impairment
Treatment approaches for hearing impairment in individuals with osteogenesis imperfecta encompass various options, including hearing aids, stapes surgery, and cochlear implants.
Stapes surgery, although effective in many cases, can lead to higher rates of postoperative hearing loss in OI patients compared to non-OI individuals. In such cases, the combination of stapedectomy with implantable hearing aids like the Vibrant SoundBridge has shown promising results in restoring hearing.
Additionally, cochlear implants and bone-anchored hearing aids are viable alternatives for managing hearing loss in individuals with OI. It's crucial to consider the specialized care requirements for OI patients undergoing stapedectomy, as the postoperative outcomes differ from those of non-OI patients.
Therefore, a tailored approach that includes close monitoring and individualized care is essential to optimize the outcomes of treatment interventions for hearing impairment in individuals with osteogenesis imperfecta.
Frequently Asked Questions
Does Osteogenesis Imperfecta Affect Hearing?
Yes, Osteogenesis Imperfecta can affect hearing. The condition's impact on hearing stems from abnormalities in collagen type I that affect inner ear structures. This can result in conductive and sensorineural hearing loss.
Prevalence rates range from 50% to 92%, with significant hearing loss often observed in individuals over 50 years old. The changes in bone structure and bony formation associated with Osteogenesis Imperfecta contribute to its effects on auditory health.
Why Does Osteoporosis Cause Hearing Loss?
Osteoporosis can lead to hearing loss due to changes in bone density affecting the delicate structures of the inner ear. The decreased bone mass can impact the transmission of sound waves, contributing to conductive hearing loss.
Additionally, osteoporosis-related bone changes may also affect the cochlea, leading to sensorineural hearing loss. The prevalence and severity of hearing loss in individuals with osteoporosis vary, necessitating appropriate diagnostic and treatment strategies like hearing aids.
What Is the Average Lifespan of Someone With Osteogenesis Imperfecta?
We've found that the average lifespan of someone with osteogenesis imperfecta can vary significantly depending on the severity of the condition.
While severe forms like Type II can be life-threatening in infancy, individuals with milder forms such as Type I or Type IV can have a closer-to-normal lifespan with proper care.
Medical advances and comprehensive management strategies have greatly improved quality of life and longevity for those with osteogenesis imperfecta.
What Parts of the Body Does Osteogenesis Imperfecta Affect?
Osteogenesis Imperfecta affects the bones, joints, teeth, and connective tissues in the body. This condition can lead to bone fragility, fractures from minor trauma, joint hypermobility, and short stature.
Additionally, individuals with Osteogenesis Imperfecta may experience hearing loss due to abnormalities in bone formation and inner ear structures. The genetic mutations associated with this condition impact type I collagen synthesis, which affects various organs including the ears.
Conclusion
In conclusion, the intricate relationship between osteogenesis imperfecta and hearing loss can be likened to a delicate symphony where genetic mutations, bone structure, collagen deficiency, and inner ear vulnerability harmonize to create a complex auditory challenge.
Despite the lack of a direct correlation between specific genes and the severity of hearing impairment in OI patients, understanding the interplay of these factors can guide treatment approaches and enhance the quality of life for individuals with this condition.