In the fast-paced world of speech therapy, some might find crafting SOAP notes to be a time-consuming task. However, mastering the art of concise and informative notes is essential for effective client care.
Have you ever wondered how a well-crafted SOAP note could not only streamline your documentation process but also improve the quality of care you provide to your clients?
Key Takeaways
- Subjective section captures client's concerns and history for effective therapy planning.
- Objective section quantifies progress and intervention effectiveness with clear observations.
- Assessment and goal setting ensure accurate progress monitoring and treatment adjustments.
- Consistent data collection and documentation support evidence-based practice and informed decision-making.
Importance of SOAP Notes
Crafting SOAP notes for speech therapy sessions holds significant importance in maintaining client progress tracking, intervention documentation, and effective communication among healthcare providers.
In speech therapy, documenting client progress through SOAP notes is crucial for tracking changes in communication abilities, treatment effectiveness, and overall well-being. These notes serve as a comprehensive record of the client's journey, detailing their challenges, achievements, and areas needing further attention.
By consistently updating SOAP notes, speech-language pathologists can monitor trends, adjust interventions as needed, and collaborate more efficiently with other healthcare professionals involved in the client's care. Additionally, these notes help in demonstrating the rationale behind treatment decisions, ensuring continuity of care, and meeting regulatory requirements.
Structure of SOAP Notes
When structuring SOAP notes for speech therapy sessions, the four main sections to include are Subjective, Objective, Assessment, and Plan. Each section plays a crucial role in documenting the client's progress and guiding future therapy sessions effectively.
Here is what each section entails:
- Subjective: This section captures client-reported concerns, mood, and relevant history, providing valuable insights into the client's perspective.
- Objective: Detailed information on therapy goals and client performance is recorded here, offering measurable data to track progress.
- Assessment: By analyzing information from the Subjective and Objective sections, therapists can evaluate progress and identify any barriers hindering development.
- Plan: Outlining the next steps for treatment, this section is essential for setting a clear path forward and achieving therapy goals efficiently.
Subjective Section
When detailing the Subjective section of a SOAP note for speech therapy, we focus on the client's presenting concerns and their therapy history. This part captures essential information like the client's current emotions, symptoms, and any changes in their condition.
Caregiver input can also play a crucial role in painting a comprehensive picture of the client's state.
Client's Presenting Concerns
Documenting the client's presenting concerns in the subjective section involves capturing pertinent information shared by the client or caregiver about the client's current state. This section provides a snapshot of the client's status at the session's onset, aiding in crafting an effective therapy plan. In this part of the SOAP note, we include details on the client's mood, recent changes in communication abilities, and any concerns expressed by the client.
Additionally, observations related to speech, language, or swallowing issues are crucial. Caregiver input, client self-reports, and relevant history are also essential components of the subjective section, allowing for a comprehensive understanding of the client's needs.
- Client's mood
- Recent changes in communication abilities
- Observations
- Caregiver input
- Relevant history
Previous Therapy History
In reviewing the client's previous therapy history, we gather essential details regarding the duration, frequency, and types of interventions utilized in past sessions. Understanding the client's previous therapy history helps us identify improvements, challenges, and changes that have occurred over time.
By documenting the client's response to previous therapy approaches, we can make necessary adjustments to the current treatment plan. This information also informs us about the effectiveness of past therapy approaches, guiding our decision-making process for the current session.
Reflecting on the client's journey through therapy provides valuable insights into their progress and helps us tailor our strategies to best meet their needs.
Objective Section

Detailing measurable information such as therapy goals, client performance, and specific observations, the Objective section in SOAP notes for speech therapy focuses on quantifying progress and intervention effectiveness. This section is crucial for tracking outcomes and assessing the effectiveness of the therapy provided.
Here are some key points to consider when documenting the Objective section:
- Include specific observations of the client's speech and language abilities.
- Document any changes in the client's condition or progress made during the session.
- Measure the client's performance against the established therapy goals.
- Record results from assessments to provide concrete evidence of improvement.
- Use clear and concise language to ensure that the information is easily understood and useful for evaluating the effectiveness of treatment strategies.
Assessment Section

When crafting SOAP notes for speech therapy sessions, it's critical to outline clear goals, establish effective data collection methods, and utilize objective measurement tools.
These elements help us monitor client progress accurately, identify areas for improvement, and make informed decisions regarding treatment strategies.
Clear Goal Setting
Crafting clear and measurable goals in the Assessment section of a SOAP note is crucial for accurately monitoring client progress in speech therapy sessions. When setting goals, it's important to consider the client's treatment plan and therapy goals. Here are key points to remember:
- Measurable objectives help assess the effectiveness of interventions.
- SMART goals ensure a structured approach to progress tracking.
- Clear goal setting guides the development of future treatment plans.
- Evaluating progress aids in adjusting treatment strategies.
- The Assessment section plays a pivotal role in determining the success of therapy sessions.
Careful goal setting in the Assessment section not only benefits the client but also enhances the overall quality of speech therapy services.
Data Collection Methods
In documenting client progress, barriers, and outcomes during speech therapy sessions, the Assessment section utilizes various data collection methods such as standardized tests, informal observations, and client performance tracking. Objective data like accuracy rates, error types, and fluency levels play a crucial role in the Assessment section.
Analysis of client responses to therapy interventions allows for adjustments to treatment plans to better suit individual needs. This section helps speech-language pathologists track client development, measure treatment effectiveness, and make informed decisions for ongoing therapy.
Objective Measurement Tools
Utilizing objective measurement tools in the Assessment section of SOAP notes for speech therapy provides precise data on clients' speech and language skills, facilitating accurate evaluation and informed decision-making.
Objective measurement tools, such as standardized tests like the CELF-5 and GFTA-3, play a crucial role in quantifying clients' progress. These tools ensure consistency and reliability in tracking development and response to therapy interventions.
Plan Section
How do we ensure that the goals outlined in the Plan section of SOAP notes are effective and measurable for the client's therapy progress?
The Plan section is crucial as it delineates the therapy goals, interventions, and treatment plan for the client. These goals should follow the SMART criteria: Specific, Measurable, Achievable, Relevant, and Time-bound. By setting SMART goals, therapists can track progress effectively, make necessary adjustments to interventions, and ultimately achieve positive client outcomes.
The Plan section acts as a roadmap for both the therapist and client, providing clear guidance on the actions needed to reach therapy objectives. It's through this section that the therapist outlines specific strategies and recommendations for ongoing therapy sessions.
Therefore, crafting well-defined and measurable goals in the Plan section is essential for guiding the therapy process and ensuring successful client progress.
Writing Effective SOAP Notes

Moving from the critical planning phase to the actual documentation of therapy sessions, crafting effective SOAP notes in speech therapy requires precision and attention to detail. When writing effective SOAP notes, it's essential to follow a consistent structure to ensure comprehensive documentation and clear communication among healthcare providers.
Here are some key points to consider:
- Subjective and Objective: Include client concerns, mood, relevant history, measurable data, therapy goals, and client performance for a holistic view.
- Assessment and Plan: Analyze information from subjective and objective sections to evaluate client development and recommend next steps for treatment.
- Measurable Data: Focus on quantifiable information to track progress effectively and make informed decisions.
- Therapy Goals: Clearly outline the objectives of the therapy sessions to guide interventions and measure client progress.
- Consistent Structure: Maintain a standardized format in your SOAP notes to ensure accuracy and continuity of care for the client's benefit.
Clear and Concise Notes
When crafting SOAP notes for speech therapy sessions, our focus is on maintaining clear and concise documentation.
Prioritizing relevant client details, progress, and treatment plans is key to effective care coordination.
Note-Taking Best Practices
Crafting clear and concise SOAP notes is essential for effective communication and documentation in speech therapy sessions. When taking notes, it's crucial to be detailed but also concise to ensure all essential information is captured accurately. Here are some best practices for note-taking:
- Use bullet points for key information.
- Avoid unnecessary details to maintain clarity.
- Organize notes into sections for easy reference.
- Focus on objective data and measurable outcomes.
- Review and edit notes to remove redundancies.
Relevant Information Prioritized
In prioritizing relevant client information within SOAP notes for speech therapy sessions, our focus is on capturing essential details that directly impact therapy outcomes. It's crucial to include client concerns, therapy goals, and measurable progress indicators in our notes.
By emphasizing key observations and interventions that are closely tied to the client's progress, we ensure that our documentation is concise and purposeful. Maintaining a structured format helps us communicate efficiently with other healthcare team members, avoiding unnecessary information that may clutter the notes.
Clear and concise note-taking is essential for tracking client development accurately and effectively. By prioritizing the most relevant information, we can tailor our interventions to better meet the needs of our clients and achieve optimal therapy outcomes.
Communication Goals Achieved
To effectively track the communication goals achieved in speech therapy sessions, we prioritize clear and concise notes that highlight specific progress indicators and measurable outcomes. When documenting therapy progress, it's crucial to focus on key aspects such as:
- Articulation: Noting improvements in speech clarity and precision.
- Fluency: Observing enhancements in speech flow and rhythm.
- Interventions: Detailing effective strategies and techniques utilized during sessions.
- Therapy Progress: Recording advancements in overall communication abilities.
- Client Responses: Documenting reactions to interventions to guide treatment planning.
Consistency in Documentation
Maintaining uniformity and accuracy in documentation is crucial for tracking client progress effectively in speech therapy. Consistency in writing SOAP notes ensures that all healthcare providers involved in the client's care are on the same page, leading to better coordination and understanding of the treatment plan. By adhering to a standardized format for documentation, such as the SOAP note structure, therapists can convey essential information clearly and concisely. This standardized approach also facilitates progress tracking over time, enabling therapists to identify trends or changes in the client's condition more easily. Consistent documentation practices not only support evidence-based practice in speech therapy but also enhance treatment planning and decision-making processes. Developing regular habits of note-taking contributes to improved client care by allowing for thorough monitoring of progress and adjustments to interventions when necessary.
| Importance of Consistency in Documentation | Benefits |
|---|---|
| Uniformity and accuracy in recording progress | Improved coordination among healthcare providers |
| Standardized format for clear communication | Enhanced progress tracking over time |
| Support for evidence-based practice | Better treatment planning and decision-making |
| Regular note-writing habits for improved client care | Thorough monitoring and intervention adjustments |
Example of a SOAP Note
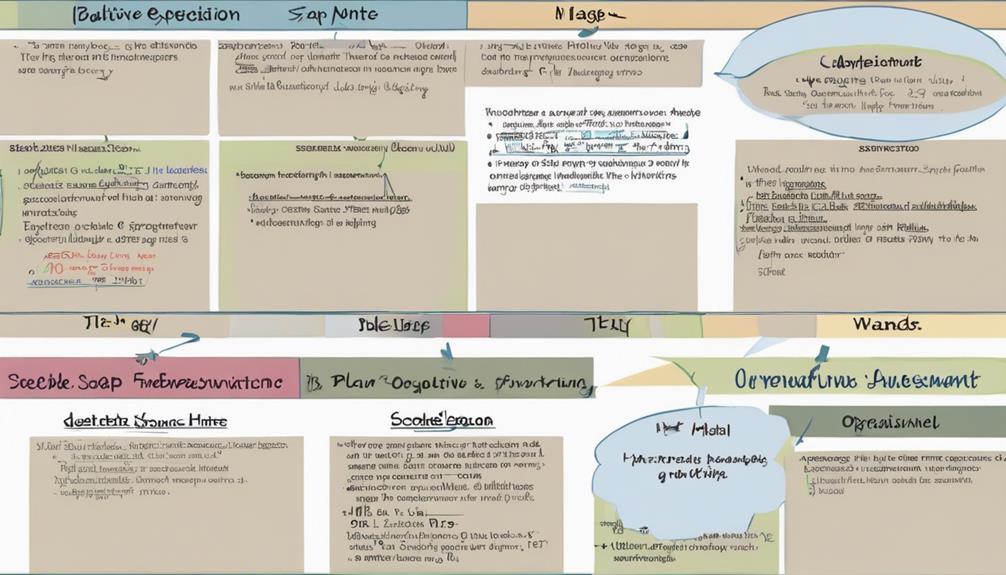
Crafting a detailed and structured SOAP note is essential for effectively documenting speech therapy sessions and tracking client progress. An example of a SOAP note for speech therapy includes subjective client concerns, objective measurable data, assessment of progress, and treatment plan details. This example showcases how to document a client's session comprehensively and efficiently.
Each section of the SOAP note demonstrates the structured format necessary for organizing information in therapy documentation. By following this example, speech therapists can clearly convey client progress, interventions, and future treatment steps. Utilizing SOAP notes in speech therapy sessions helps track client development, communicate with other healthcare providers, and ensure effective treatment planning.
- Subjective client concerns
- Objective measurable data
- Assessment of progress
- Treatment plan details
- Structured format for organizing information
Benefits of EMR Software

Transitioning from documenting speech therapy sessions to discussing the benefits of EMR software, we explore how electronic medical records streamline administrative tasks, enhance efficiency, and ensure secure storage of client data. EMR software plays a crucial role in speech therapy practices by simplifying note-taking processes, thus saving time and improving accuracy in documentation.
When integrated with practice management software, EMR systems further boost efficiency, allowing therapists to focus more on patient care. The use of electronic records guarantees secure storage and easy access to client notes and treatment plans, promoting better continuity of care.
Frequently Asked Questions
Why Use Crafts in Speech Therapy?
Crafts are valuable in speech therapy for their ability to enhance engagement, motivate clients, and target various speech and language goals creatively. They offer hands-on opportunities for communication practice and can improve fine motor skills while addressing speech objectives simultaneously.
The multisensory approach of crafts makes learning more enjoyable, providing a fun and functional way for clients to work on their skills.
How Do You Write Effective SOAP Notes?
When we write effective SOAP notes, we aim to capture client progress accurately. We include subjective observations and measurable data to create a comprehensive picture. Analyzing this information helps us identify barriers and plan next steps.
Consistency in documentation is key for tracking development and ensuring continuous care. The process involves attention to detail, clarity, and a client-centered approach to serve others effectively.
What Is the Subjective Section of a SOAP Note for Speech Therapy?
In speech therapy, the subjective section of a SOAP note captures the client's concerns, mood, and relevant history from their viewpoint. Caregiver input, client self-reports, and observations shape this part of the note, providing a comprehensive overview.
Documenting medications, recent events, and emotional states lays the foundation for the rest of the SOAP note, offering context and focusing on the client's experiences and needs during the session.
What Not to Include in SOAP Notes?
When writing SOAP notes, we must avoid including personal opinions, irrelevant details, sensitive information, technical jargon, and unsupported assumptions. By adhering to these guidelines, we ensure that our documentation remains focused on the client's progress and is clear to all readers.
Following this approach helps maintain professionalism and accuracy in our records, ultimately benefiting the client's therapy journey. Remember, less is more when it comes to effective documentation.
Conclusion
In conclusion, crafting effective SOAP notes for speech therapy sessions is essential for providing quality care and documenting client progress. These notes serve as a roadmap for therapy goals, evaluation of progress, and treatment plans.
By maintaining consistency, utilizing tools like EMR software, and ensuring clear and concise documentation, speech-language pathologists can enhance communication with healthcare providers and support evidence-based practice for optimal client outcomes.
Just like a well-crafted painting, meticulous attention to detail in SOAP notes can truly make a difference in client care.











