Curious to uncover the unexpected connection between meningitis and hearing loss? Let’s explore how this infection impacts our ability to hear in a intricate way.
From the underlying mechanisms to potential long-term consequences, understanding this relationship is crucial for both medical professionals and individuals alike.
So, are you ready to unravel the mysteries of how meningitis can lead to hearing impairment?
Key Takeaways
- Bacterial meningitis damages auditory structures, causing sensorineural hearing loss.
- Children are particularly vulnerable to cochlear hair cell and auditory nerve damage post-meningitis.
- Severity of post-meningitis hearing loss varies, affecting speech and social development.
- Early detection, intervention, and regular monitoring are crucial for managing meningitis-related hearing loss.
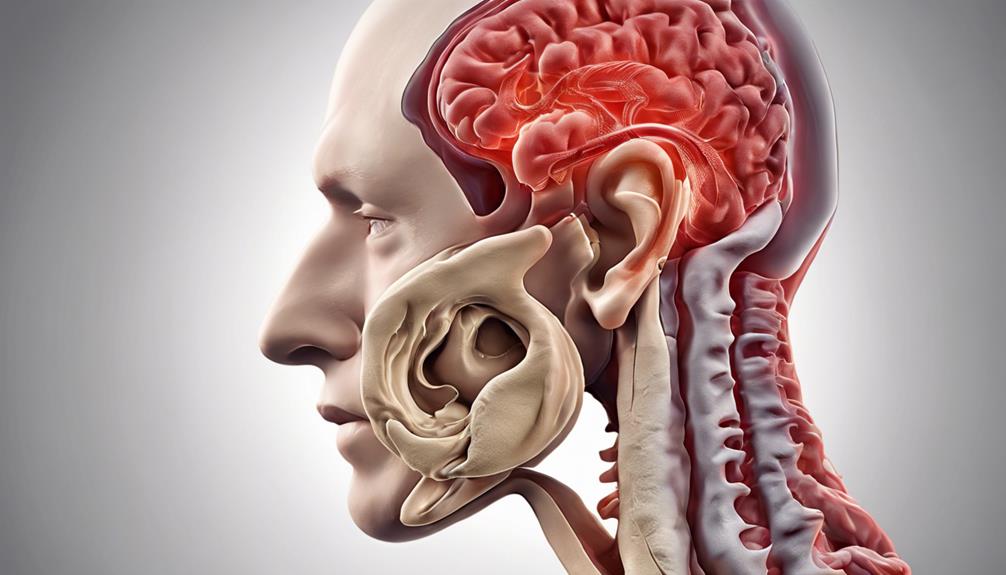
Understanding Meningitis-Related Hearing Loss
Bacterial meningitis poses a serious risk of causing sensorineural hearing loss by damaging the inner ear's auditory structures. In children, the cochlea's delicate hair cells can be affected by the inflammation and bacterial toxins from the infection, leading to impaired hearing. This damage extends to the auditory nerve, causing sensorineural deafness post-meningitis. The severity of hearing loss can vary from mild to profound, impacting speech and social development in affected individuals. The intricate components of the inner ear are particularly vulnerable to the harmful effects of bacterial meningitis, emphasizing the importance of early detection and intervention.
Understanding the mechanisms through which meningitis can result in hearing loss is crucial for effectively managing this potential complication. By recognizing the intricate connection between bacterial meningitis and damage to the auditory structures, healthcare providers can implement timely interventions to mitigate the long-term consequences of sensorineural hearing loss in meningitis survivors. Vigilant monitoring and proactive measures are essential in safeguarding the auditory health of individuals who've experienced bacterial meningitis.
Causes and Risk Factors

After exploring the detrimental impact of bacterial meningitis on hearing loss, it is crucial to delve into the specific causes and risk factors associated with this complication. Streptococcus pneumoniae and Neisseria meningitidis are pathogens commonly implicated in hearing loss post-bacterial meningitis. Factors such as young age, severity of symptoms, delayed treatment, and certain cerebrospinal fluid substances increase the risk of developing hearing impairment following bacterial meningitis. In high-income countries, 14-32% of children with pneumococcal meningitis experience hearing loss. On the other hand, viral meningitis rarely leads to hearing impairment, while fungal and parasitic meningitis have lower chances of causing hearing loss. Sensorineural hearing loss from meningitis can be attributed to cochlear ossification, inner ear nerve damage, and auditory nerve cell death. Understanding these causes and risk factors is vital for early detection and appropriate management of meningitis-related hearing loss.
| Causes | Risk Factors | Associated Pathogens |
|---|---|---|
| Cochlear ossification | Young age | Streptococcus pneumoniae |
| Inner ear nerve damage | Severity of symptoms | Neisseria meningitidis |
| Auditory nerve cell death | Delayed treatment |
Pathology and Diagnosis
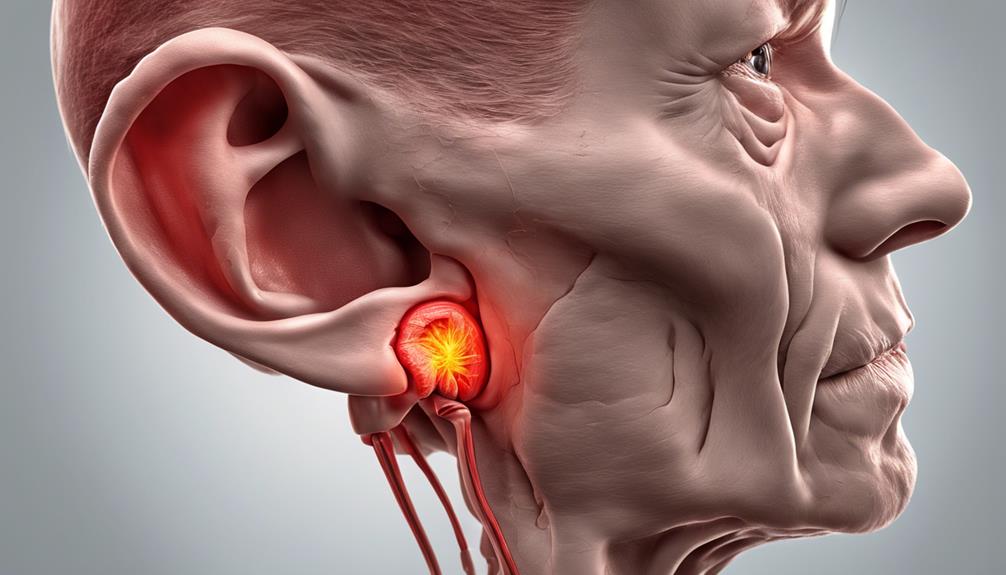
Exploring the pathology and diagnosis of meningitis-related hearing loss reveals crucial insights into the mechanisms and assessment methods for this complication. Meningitis can lead to sensorineural hearing loss by damaging inner ear nerve fibers and cochlear hair cells. The impact of septicemia from bacterial meningitis can result in cell death within the inner ear and auditory nerve, further contributing to hearing loss. Additionally, cochlear ossification, characterized by the transformation of cochlear fluid into bone, can exacerbate hearing loss following a meningitis infection.
Diagnosis of meningitis-related hearing loss typically involves otoscopic examination, audiologist-performed tests, and imaging to assess potential cochlear damage. Detecting this condition early is vital for effective management of potential hearing loss complications. Therefore, regular post-meningitis hearing tests play a crucial role in monitoring and addressing any changes in auditory function that may arise.
Audiologist Procedures and Testing Recommendations

When assessing individuals for meningitis-related hearing loss, audiologists employ a range of procedures and testing recommendations to evaluate auditory function effectively. To ensure a comprehensive assessment, audiologists use otoscopes to examine the ear for fluid and conduct behavioral tests such as BOA, VRA, and CPA for hearing assessment.
Additionally, various auditory function tests, including pure-tone testing, bone conduction testing, and ABR, are performed to measure hearing sensitivity and ear function post-meningitis. In cases where cochlear ossification is suspected, imaging tests like MRI or CT scans may be recommended.
It's crucial that infants, children, teens, and adults who've had meningitis undergo post-infection hearing tests to monitor and manage any resulting hearing loss. Regular follow-up testing is essential for evaluating the impact of meningitis on hearing and determining the necessity of interventions like hearing aids or cochlear implants for effective hearing loss management.
Treatment and Prevention
Our focus now shifts to discussing the strategies for treating and preventing meningitis-related hearing loss. Vaccination plays a critical role in prevention, with vaccines such as Hib, pneumococcal, Meningococcal conjugate, and MenB being essential. These vaccines help reduce the risk of contracting meningitis, thus lowering the chances of associated hearing loss.
In cases where hearing loss does occur post-meningitis, various interventions can help manage the condition. Hearing aids, ranging from in-the-ear to behind-the-ear devices, are effective in addressing most instances of hearing impairment. For severe sensorineural hearing loss, cochlear implants offer a solution for improved quality of life and restored hearing abilities.
Additionally, speech therapy and auditory-verbal therapy can be beneficial in assisting individuals in coping with hearing loss post-meningitis. Early detection of meningitis, coupled with prompt treatment and vaccination, remains crucial in preventing and mitigating the impact of hearing loss linked to this disease. By employing these strategies, individuals can take proactive steps towards maintaining their auditory health.
Frequently Asked Questions
How Does Meningitis Cause Hearing Loss?
Meningitis causes hearing loss by damaging inner ear structures like the cochlea's hair cells. Inflammatory responses and bacterial toxins lead to inner ear damage, affecting hearing.
Post-meningitis, sensorineural hearing loss is common due to cochlear nerve and hair cell damage, impacting one or both ears. The severity of hearing loss can range from mild to profound.
Early detection, treatment, and follow-up testing are crucial for effective management.
Can Meningitis Cause Auditory Processing Disorder?
Yes, meningitis can indeed cause auditory processing disorder (APD). This disorder stems from damage to the auditory pathways due to meningitis.
APD can manifest as challenges in understanding speech, especially in noisy settings, and following instructions. It necessitates distinct diagnostic tests for accurate evaluation.
Early identification and intervention post-meningitis can significantly enhance communication and learning outcomes.
What Are the 5 Causes of Meningitis?
Meningitis, a serious condition, can have various causes. Bacterial infections by pathogens like Streptococcus pneumoniae and Neisseria meningitidis are common culprits. Additionally, viral infections, brain surgery, certain medications, or non-infectious factors can lead to this illness.
Streptococcus pneumoniae is linked to significant cases of hearing loss post-meningitis. In children from high-income countries, pneumococcal meningitis can result in hearing loss in a notable percentage of cases.
Can Meningitis Cause Blindness and Deafness?
Blindness is a possibility with meningitis, but what about deafness? Yes, it can occur. The infection can harm the inner ear, leading to hearing loss. Cochlear damage and nerve impairment can result in profound deafness.
Swift detection and treatment are vital for managing post-meningitis hearing loss. It's crucial to monitor and intervene early to address any potential auditory issues caused by this serious infection.
Conclusion
As we've seen, meningitis can sneak up on us and steal our hearing without warning. Despite advances in treatment and monitoring, the damage done by this disease can be irreversible.
So next time you hear someone say they're not worried about meningitis, maybe remind them that silence isn't always golden. Stay vigilant, stay informed, and protect your ears – you never know when they might be at risk.