Living with Hearing Loss
You Can Get Disability for Being Deaf in One Ear
Curious about disability benefits for unilateral deafness? Explore the intricate criteria and application process that can shape your journey.

Navigating through the world of disability benefits for unilateral deafness can feel like exploring a complicated maze with its own set of rules and criteria.
The intricacies of qualifying for support when experiencing deafness in one ear can be puzzling, but fear not, for we are here to shed light on this matter.
From understanding the eligibility requirements to the application process and the impact on daily life, there are crucial aspects to explore in this realm.
So, let's unravel the layers of how being deaf in one ear can potentially shape your journey towards securing necessary assistance.
Key Takeaways
- Meeting specific criteria for profound hearing loss in one ear is crucial.
- Documenting functional limitations on daily activities and work performance is essential.
- Seeking legal guidance can help navigate the application process effectively.
- Demonstrating the impact of deafness on quality of life increases chances of approval.
Understanding Disability Benefits for Unilateral Deafness
Understanding the criteria for disability benefits related to unilateral deafness is crucial for individuals seeking financial support for their condition. When it comes to qualifying for disability benefits due to deafness in one ear, meeting specific requirements for profound hearing loss in that ear is paramount. The SSA Listing for hearing outlines the thresholds for profound hearing loss that make individuals eligible for benefits. It's important to note that even individuals with good hearing in one ear may still qualify for disability benefits based on the impact unilateral deafness has on their daily life and work.
Documenting the severity and functional impact of unilateral deafness is essential for a successful disability claim approval. Providing detailed evidence of how deafness in one ear hinders communication, job performance, and overall quality of life strengthens the case for benefit eligibility. Seeking legal guidance during the application process can help navigate the complexities of proving the extent of the disability and increase the chances of a successful claim.
Eligibility Criteria for Deafness in One Ear

When determining eligibility for disability benefits due to deafness in one ear, it's crucial to meet Social Security's requirements by providing detailed medical evidence of profound hearing loss. Documenting the impact of limited functional capacity resulting from one-sided deafness is essential for qualification.
Even individuals with partial hearing in one ear may be eligible if they can demonstrate significant limitations affecting their daily activities and work performance.
One-Sided Deafness Criteria
Individuals with one-sided deafness may qualify for disability benefits based on specific eligibility criteria related to the impairment of hearing in one ear. When assessing eligibility for disability benefits due to one-sided deafness, the Social Security Administration (SSA) considers the following criteria:
- Functional Limitations: The impact of hearing loss in one ear on an individual's ability to effectively communicate and function in work settings.
- Severity of Impairment: Meeting the SSA's listing of impairments for hearing loss in one ear, which requires demonstrating the inability to carry out daily activities and job tasks effectively.
- Daily Life and Job Performance: Individuals with severe hearing loss in one ear may be eligible for disability benefits based on the significant impact on their daily activities and job performance.
Hearing Loss Documentation
Hearing loss documentation required for disability benefits necessitates audiometric testing conducted by a licensed audiologist to determine eligibility criteria for deafness in one ear. Specific tests like word recognition tests are essential to showcase the severity of hearing loss. The Social Security Administration (SSA) may request medical evidence from an otolaryngologist and additional tests to support the disability claim. Cochlear implantation is a factor considered during disability determination for individuals experiencing hearing loss. Meeting the official SSA listing criteria for hearing loss requires specific tests and documentation to establish eligibility.
| Audiometric Testing | Word Recognition Test |
|---|---|
| Determines hearing levels | Assesses ability to understand speech |
| Conducted by audiologist | Crucial for demonstrating severity of hearing loss |
Application Process for Disability Benefits
Gathering comprehensive medical records that support the claim is a crucial initial step in the application process for disability benefits due to being deaf in one ear. When applying for disability benefits, attention to detail is key. Here are essential steps to follow:
- Accurate Application Completion: Ensure the disability benefits application is filled out accurately and thoroughly. Any missing information could delay or hinder the approval process.
- Consultation with Healthcare Providers: Seek documentation from healthcare providers that clearly outlines the extent of your hearing loss. Detailed medical records can significantly strengthen your disability benefits application.
- Legal Assistance: Consider seeking legal assistance to navigate the complexities of the application process. Legal professionals can offer guidance on what documentation is necessary and can help ensure that the application is correctly filled out.
Impact of Unilateral Deafness on Daily Life

Navigating daily activities can pose significant challenges for individuals with unilateral deafness, impacting spatial awareness and communication abilities in various settings. Unilateral deafness can lead to difficulties in accurately determining the source and distance of sounds, affecting the ability to localize sounds and maintain spatial awareness.
In noisy environments, individuals with deafness in one ear may struggle to filter out background noise, making it challenging to focus on specific sounds and conversations. Communication challenges are also prevalent, especially in group settings where following conversations can be arduous.
Tasks like driving, crossing the street, and participating in team sports may require extra caution and attention for individuals with unilateral deafness due to limitations in auditory information. The emotional effects of unilateral deafness can include feelings of isolation and frustration in social interactions, highlighting the need for support systems that address both the practical and emotional aspects of living with this condition.
Support Available for Individuals With Hearing Loss

We can explore the various support options available for individuals experiencing hearing loss, particularly those with unilateral deafness.
- Social Security Disability Insurance (SSDI):
SSDI may provide essential support for individuals with profound hearing loss in one ear. Qualifying for SSDI benefits requires meeting specific eligibility criteria, including audiometry tests to assess the severity of the hearing loss.
- Legal Assistance:
Seeking legal assistance can be crucial in navigating the application process for disability benefits related to hearing loss. Legal professionals can provide guidance on the necessary documentation and ensure that all requirements are met for a successful claim.
- Disability Benefits:
Individuals seeking benefits for deafness in one ear must demonstrate how it significantly impacts their ability to work and engage in daily activities. Properly documenting the effects of unilateral deafness is essential for approval and receiving the necessary support.
Cochlear Implant Considerations for Disability

Individuals with unilateral deafness may find that cochlear implants play a pivotal role in determining their eligibility for disability benefits. Cochlear implants can indicate profound hearing loss, which is a key factor in supporting a claim for disability benefits.
The Social Security Administration considers cochlear implantation as part of the eligibility criteria for disability benefits. In some cases, meeting specific criteria with cochlear implants can lead to automatic approval for these benefits.
After cochlear implantation, individuals may qualify for disability benefits for a year. However, to continue receiving benefits beyond the initial year, additional impairments may need to be present to meet the eligibility criteria.
Understanding the role of cochlear implants in the context of disability benefits is crucial for individuals with unilateral deafness seeking financial support. The decision to pursue cochlear implants not only impacts their hearing health but also their potential eligibility for disability benefits.
Medical Evidence Required for Deafness Claims

When establishing deafness claims, the medical evidence required typically involves audiometric testing conducted by a licensed audiologist. To support a deafness claim effectively, the following steps are crucial:
- Audiometric Testing: This initial testing assesses the extent of hearing loss and is a fundamental component in providing evidence for a deafness claim.
- Otolaryngologist Examination: A physical examination by an otolaryngologist is essential to evaluate the severity of the hearing impairment and determine its impact on daily functioning.
- Auditory Evoked Response Testing: In certain cases, auditory evoked response testing may be necessary to provide comprehensive evidence supporting the deafness claim.
Meeting the Social Security Administration's listing for deafness requires a meticulous approach to gathering medical evidence. This includes adherence to specific tests and documentation standards outlined in the SSA listing for deafness.
Meeting the SSA Listing for Unilateral Deafness

When aiming to meet the SSA listing for unilateral deafness, it's essential to focus on the specific criteria outlined by the Social Security Administration.
Gathering comprehensive medical evidence that showcases the extent of limitations caused by unilateral deafness is crucial for a successful disability claim.
Understanding the requirements and ensuring that the evidence presented aligns with the SSA criteria is fundamental in pursuing disability benefits for unilateral deafness.
SSA Listing Criteria
Meeting the SSA listing for unilateral deafness necessitates a pure-tone average of 90 decibels or higher in the better ear. When evaluating unilateral deafness for disability benefits, the SSA considers various factors to determine eligibility.
Here are key points to understand regarding the SSA listing criteria for unilateral deafness:
- Pure-Tone Average Requirement: A pure-tone average of 90 decibels or higher in the better ear is necessary to meet the SSA listing criteria for unilateral deafness.
- Speech Discrimination Scores: Individuals with deafness in one ear may also qualify if their speech discrimination scores fall below a specific threshold.
- Impact Assessment: The impact of unilateral deafness on daily activities and communication abilities is carefully assessed by the SSA to determine eligibility for disability benefits.
Medical Evidence Required
To establish eligibility for disability benefits due to unilateral deafness, comprehensive medical evidence, including audiometric testing conducted by a licensed audiologist, is essential. Specific tests such as pure-tone audiometry and speech discrimination testing play a crucial role in documenting the extent of hearing loss in one ear. Additionally, auditory evoked response testing may be necessary to provide further support for the claim of unilateral deafness.
Meeting the official SSA listing criteria for unilateral deafness requires demonstrating not only significant hearing loss but also the functional limitations it imposes. Therefore, a detailed medical report outlining the impact of unilateral deafness on daily activities and work is vital for the approval of disability benefits. This evidence is indispensable in showcasing the severity of unilateral deafness and its effects on an individual's life.
Functional Capacity Assessment for Hearing Loss

Functional capacity assessments for hearing loss involve analyzing an individual's ability to engage in daily activities and work tasks, determining the impact of hearing impairment on various functions. When conducting these assessments, several key points are considered:
- Residual Functional Capacity: This rating is crucial and is determined based on the severity of the hearing impairment and its associated limitations. It reflects the individual's remaining ability to function in a work environment.
- Work Restrictions: Based on the results of the functional capacity assessment, specific work restrictions may be recommended to accommodate the individual's hearing impairment and ensure a safe and productive work environment.
- Job Availability Evaluations: These evaluations take into account the individual's residual functional capacity, along with factors such as age, education, and work experience, to assess the types of jobs that may be suitable for the individual given their hearing impairment.
Importance of Using Qualified Interpreters
Using qualified interpreters is essential to ensure accurate and effective communication during the disability application process. Interpreter certification plays a critical role in guaranteeing the quality of interpretation provided to deaf or hard of hearing individuals.
Understanding communication access rights and the importance of high-quality interpretation is fundamental in accurately conveying the impact of hearing loss on daily life and work functions.
Interpreter Certification Importance
Ensuring certification of interpreters is paramount to guaranteeing accurate and effective communication for individuals with hearing impairments during disability claim processes.
Importance of Interpreter Certification:
- Proficiency in Sign Language: Certified interpreters possess advanced skills in sign language, ensuring precise translation of information.
- Understanding of Deaf Culture: Certification includes knowledge of deaf culture, enhancing the interpreter's ability to convey nuances effectively.
- Legal and Medical Expertise: Certified interpreters are trained to handle complex legal and medical terminology, aiding in accurate communication during disability claim proceedings.
Certified interpreters play a crucial role in bridging communication gaps for individuals with hearing loss, ensuring fair treatment and access to disability benefits from organizations like the Social Security Administration.
Communication Access Rights
Deaf or hard of hearing individuals have the right to demand a qualified sign language interpreter to ensure effective communication. Utilizing a qualified interpreter is crucial for accurately conveying information, especially during the disability benefits application process. Sign language interpreters provided by Social Security enable equal access to services for all applicants, ensuring deaf individuals receive the same opportunities as hearing applicants. Clearly articulating how hearing loss impacts daily life outside of work is vital when initiating a disability claim. By advocating for communication access rights, individuals with hearing loss can navigate the application process more effectively and secure the benefits they deserve.
| Communication Access Rights | Importance |
|---|---|
| Qualified Sign Language Interpreter | Ensures effective communication |
| Social Security Services | Offer free interpreters for equal access |
| Accuracy | Vital during benefits application |
| Equal Opportunities | Deaf and hearing applicants |
| Articulation of Hearing Loss Impact | Crucial for disability claims |
Quality of Interpretation
Transitioning from the discussion on Communication Access Rights, we emphasize the critical role of utilizing qualified interpreters to ensure accurate communication in disability claims involving individuals with hearing loss.
- Qualified Interpreters Ensure Accuracy: Using a qualified interpreter is crucial for conveying information accurately between the applicant and the Social Security Administration.
- Full Participation: Qualified interpreters guarantee that individuals with hearing loss can actively participate in the application process, securing their right to equal treatment.
- Right to Access: Access to a qualified sign language interpreter is a fundamental right for individuals who are deaf or hard of hearing, ensuring they receive fair consideration during the disability benefits application process.
Sign Language Skills for Disability Claims

Mastering sign language can significantly enhance the effectiveness of disability claims filed in relation to deafness in one ear. When individuals possess strong sign language skills, they can effectively navigate communication barriers caused by their hearing impairment. By showcasing proficiency in sign language, claimants provide concrete examples of the functional limitations they experience due to their deafness in one ear. Sign language fluency serves as a powerful tool in illustrating the impact of hearing loss on daily interactions, highlighting the challenges faced in various settings.
In the context of disability claims, the ability to communicate through sign language not only demonstrates the severity of the impairment but also showcases the efforts made to overcome obstacles. Utilizing sign language in these claims adds a layer of authenticity and clarity, allowing adjudicators to grasp the full extent of the communication barriers faced by individuals with unilateral deafness. Overall, incorporating sign language skills into disability claims can significantly strengthen the case presented and provide a more comprehensive understanding of the claimant's situation.
Starting a Disability Claim for Unilateral Deafness

When initiating a disability claim for unilateral deafness, it's essential to gather comprehensive medical evidence that clearly delineates the severity and functional impact of the hearing impairment on daily activities and occupational performance.
Here are three key steps to consider:
- Document Hearing Loss: Provide detailed medical records, including audiograms and assessments from healthcare professionals, to demonstrate the extent of hearing loss in one ear.
- Describe Functional Limitations: Clearly articulate how unilateral deafness affects communication, spatial awareness, and overall job performance to strengthen your case for disability benefits.
- Meet SSA Criteria: Ensure that your medical evidence aligns with the Social Security Administration's guidelines for unilateral deafness to facilitate a smoother approval process for disability benefits.
Securing Deserved Compensation for Hearing Loss

Securing deserved compensation for hearing loss requires thorough documentation of the functional limitations caused by deafness in one ear and meeting specific medical criteria essential for eligibility. Individuals seeking disability benefits due to deafness in one ear must demonstrate the significant impact on their ability to work and perform daily activities.
The severity and consequences of hearing loss in one ear play a crucial role in determining eligibility for disability compensation. Detailed documentation outlining how deafness in one ear affects communication, spatial awareness, and overall quality of life is vital in the application process. Providing evidence of these functional limitations is key to justifying the need for disability support.
Seeking legal guidance can help navigate the complexities of the application process and increase the chances of securing the deserved compensation for hearing loss in one ear. By following the necessary steps and meeting the specific medical criteria, individuals can enhance their prospects of receiving the disability benefits they're entitled to.
Frequently Asked Questions
Is Being Deaf in 1 Ear a Disability?
Being deaf in one ear can indeed qualify as a disability, depending on its impact on daily life and work. The Social Security Administration considers unilateral deafness as a disabling condition, requiring documentation of severity and functional limitations for approval.
Meeting specific medical criteria is crucial for eligibility. It's essential to demonstrate how deafness in one ear significantly impairs one's ability to function in various aspects of life to qualify for disability benefits.
Can You Claim Disability for Being Deaf in One Ear?
Yes, we can claim disability for being deaf in one ear if it significantly impairs daily function and work. Severity and impact are vital considerations for qualification. Meeting SSA criteria for hearing loss is key.
Documenting how single-sided deafness affects communication and work tasks strengthens claims. Seeking medical evaluation and supporting evidence are crucial.
Eligibility hinges on the condition's impact on daily life and ability to work.
What Is a Disability With No Hearing in One Ear?
Having no hearing in one ear can be deemed a disability if it significantly impacts daily life and work capabilities. Unilateral deafness poses challenges in spatial awareness, communication, and hearing in noisy environments. It affects balance, sound localization, and directional hearing.
This condition can qualify as a disability due to its impact on work performance and social interactions. Seeking medical evaluation is crucial for determining disability eligibility based on unilateral deafness.
What Happens if You Are Deaf in One Ear?
Being deaf in one ear can impact daily life in various ways. Communication challenges, difficulty localizing sounds, and potential safety issues are common.
Understanding speech in noisy environments might be problematic. Seeking medical advice and potential accommodations can help manage these difficulties.
Collaboration with healthcare providers and utilizing assistive devices can improve quality of life for those experiencing deafness in one ear.
Can a Person with Unilateral Deafness Qualify for Disability Benefits?
Yes, a person with unilateral deafness may qualify for disability benefits, depending on the severity of their condition and how it impacts their ability to work. Some people with unilateral deafness may experience challenges in certain professional settings, such as deaf gynecologist examinations techniques.
Can Deafness in One Ear Impact a Lawyer’s Ability to Practice Law?
Yes, deaf lawyers in the legal field can face challenges related to their ability to hear crucial information during court proceedings and client interactions. However, accommodations such as visual aids and assistive technology can help mitigate the impact of deafness in one ear on a lawyer’s ability to practice law effectively.
Conclusion
In conclusion, navigating the process of obtaining disability benefits for unilateral deafness requires meticulous attention to medical evidence and documentation.
Like a skilled navigator charting a course through turbulent waters, individuals must advocate for themselves and seek the support they need to secure the compensation they deserve.
By following the proper steps and utilizing available resources, individuals with hearing loss can access the assistance they need to improve their quality of life.
Jamie is one of the creative forces behind the words that resonate with our audience at Deaf Vibes. With a passion for storytelling and advocacy, Jamie delves into topics that matter deeply to the deaf and hard-of-hearing community. Jamie’s articles are crafted with empathy, insight, and a commitment to positive change, from exploring the latest advancements in hearing technologies to shedding light on the everyday challenges and victories of those within the community. Jamie believes in the power of shared stories to inspire action, foster understanding, and create a more inclusive world for everyone.
Understanding Hearing Loss
How Does Tobramycin Cause Hearing Loss? A Guide
Journey into the intricate connection between tobramycin and hearing loss to uncover the surprising ways it impacts our ears.
In terms of the impact of tobramycin on hearing loss, its importance may be underestimated.
Have you ever wondered how this common antibiotic can lead to potential damage in our ears?
Let's explore the intricate mechanisms behind tobramycin-induced hearing impairment and uncover the essential insights that can help us better understand and potentially mitigate this side effect.
Key Takeaways
- Tobramycin damages inner ear hair cells, leading to irreversible hearing loss.
- Genetic factors increase susceptibility to tobramycin-induced ototoxicity.
- Hair cell damage pathways involve disruption of essential cellular processes.
- Monitoring drug levels and genetic predispositions are crucial in preventing hearing loss.
Tobramycin's Mechanism of Ototoxicity
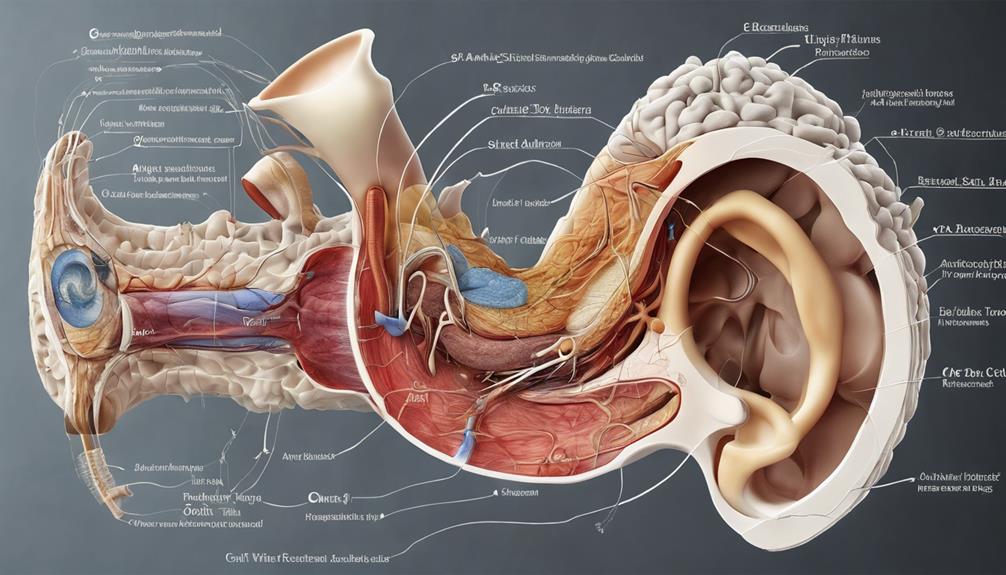
Tobramycin exerts its ototoxic effects by directly damaging the delicate hair cells within the inner ear, causing significant impairment in auditory function. This damage occurs primarily in the cochlea, a spiral-shaped structure responsible for converting sound vibrations into electrical signals that the brain can interpret. The inner ear houses sensory cells crucial for hearing, including the hair cells that detect sound waves and transmit signals to the auditory nerve. When tobramycin interferes with these hair cells, it can lead to permanent hearing loss.
The inner ear's intricate architecture makes it particularly vulnerable to the toxic effects of tobramycin. The drug disrupts the normal functioning of these hair cells, ultimately resulting in their degeneration and loss. Once these cells are damaged, they're unable to regenerate, leading to irreversible hearing impairment. This profound impact on the inner ear underscores the importance of monitoring tobramycin usage carefully, especially in individuals with genetic predispositions or mitochondrial DNA mutations that heighten susceptibility to ototoxicity.
Impact on Auditory Hair Cells
Damage to the delicate auditory hair cells in the inner ear is a critical consequence of tobramycin exposure, often resulting in irreversible hearing loss. Tobramycin, commonly used to treat infections like otitis media, exerts its ototoxic effects by directly damaging the sensory cells in the cochlea. This damage leads to sensorineural hearing loss, affecting the ability to perceive sound accurately. The side effects of tobramycin on auditory hair cells can have profound implications for individuals undergoing treatment with this medication, highlighting the importance of monitoring hearing function during therapy.
Understanding the specific pathways through which tobramycin impacts auditory hair cells is an active area of research. Researchers are working to elucidate the mechanisms involved in the toxicity of tobramycin to develop strategies that can mitigate or prevent hearing loss associated with its use. By unraveling the intricate processes through which tobramycin damages auditory hair cells, scientists aim to improve treatment outcomes and minimize the risk of irreversible hearing impairment for patients receiving this medication.
Genetic Factors in Hearing Loss
In understanding the potential genetic factors contributing to hearing loss, researchers have identified specific genetic markers and mitochondrial DNA mutations that can increase susceptibility to aminoglycoside-induced ototoxicity. Genetic susceptibility is a crucial aspect in the development of drug-induced hearing loss, particularly with ototoxic medications like tobramycin.
Here are key points to consider:
- Certain genetic factors and mitochondrial DNA mutations can predispose individuals to aminoglycoside ototoxicity, including hearing loss.
- Genetic susceptibility plays a significant role in drug-induced hearing loss associated with ototoxic medications like tobramycin.
- Patients with specific genetic predispositions require closer monitoring when using ototoxic medications to prevent hearing damage.
Mitochondrial DNA abnormalities are known to contribute to the risk of aminoglycoside-induced hearing loss. Avoiding ototoxic antibiotics in individuals with genetic susceptibility is essential to prevent permanent hearing impairment. Understanding these genetic factors is essential in personalized medicine approaches to mitigate the risk of ototoxicity and preserve hearing function.
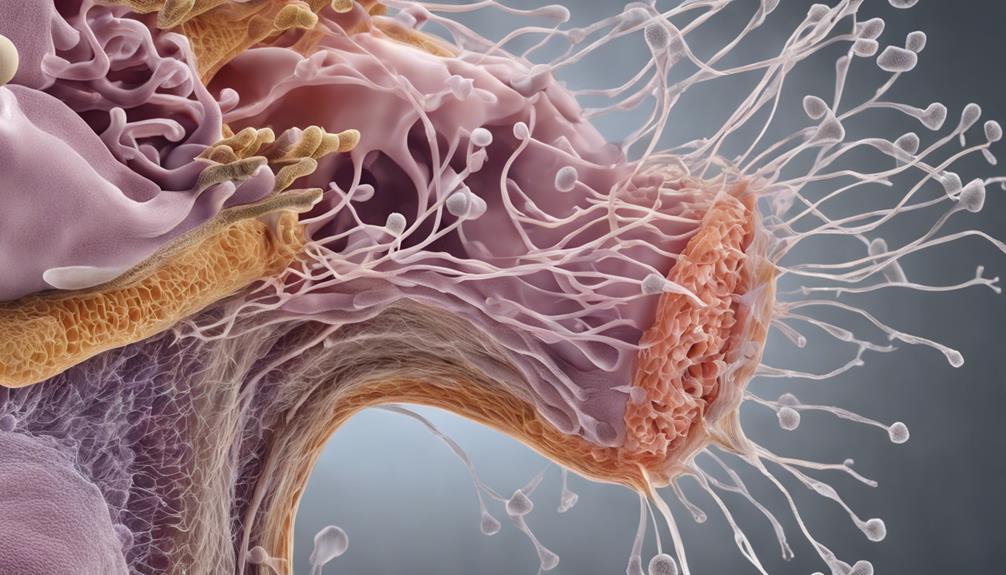
Pathways of Ototoxic Hair Cell Damage

Among the mechanisms underlying ototoxic hair cell damage, a key pathway involves the disruption of crucial cellular processes essential for auditory function. Tobramycin, through its toxic effects on the cochlea, interferes with the maintenance of hair cell integrity and function. This disruption can lead to the degeneration and death of these sensory cells, resulting in sensorineural hearing loss.
The severity of tobramycin-induced hair cell damage can vary depending on factors such as dosage and duration of exposure. High-frequency hearing loss is a common manifestation of tobramycin ototoxicity, impacting the perception of sounds in the higher range. Both ears are typically affected by tobramycin-induced cochlear toxicity, contributing to bilateral hearing impairment.
Understanding the pathways through which tobramycin causes ototoxic hair cell damage is crucial in developing strategies to mitigate its severe side effects on hearing.
Strategies for Hair Cell Protection
Exploring proactive measures to safeguard hair cells from tobramycin-induced hearing impairment involves strategic considerations such as minimizing dosage, closely monitoring medication levels, and assessing genetic predispositions.
When aiming to protect hair cells from tobramycin's ototoxic effects, several key strategies can be implemented:
- Minimize Dosage: Utilize the lowest effective dosage of tobramycin to reduce the risk of ototoxicity and potential damage to hair cells.
- Monitor Medication Levels: Regularly monitor tobramycin levels, especially in individuals with compromised kidney function, to adjust dosages accordingly and mitigate ototoxic effects.
- Assess Genetic Predispositions: Consider genetic factors and mitochondrial DNA mutations that may predispose individuals to tobramycin-induced ototoxicity. Close monitoring is crucial in such cases to prevent irreversible damage to hair cells.
Frequently Asked Questions
Does Tobramycin Cause Hearing Loss?
Yes, tobramycin can cause hearing loss. It's important to monitor for signs like tinnitus, dizziness, and hearing impairment when taking this medication. Factors like dosage, treatment duration, and existing health conditions can increase the risk.
Genetic factors and mitochondrial DNA mutations may also play a role in susceptibility to tobramycin-induced ototoxicity. Being aware of these factors and closely monitoring for symptoms are crucial when using this antibiotic.
Can Tobramycin Eye Drops Cause Ototoxicity?
Yes, tobramycin eye drops can cause ototoxicity, leading to hearing loss. While the risk is lower than with systemic use, it's still a concern.
Symptoms may include hearing loss, tinnitus, and balance issues. Following prescribed usage and promptly reporting any unusual symptoms to a healthcare provider is crucial for preventing ototoxicity.
It's essential to be vigilant and proactive in monitoring for these potential side effects.
Can You Get Ototoxicity From Inhaled Tobramycin?
Yes, ototoxicity can occur from inhaled tobramycin, potentially resulting in hearing loss and balance issues. However, the risk is generally lower when compared to systemic administration.
It's vital to monitor for any signs of hearing impairment while undergoing inhaled tobramycin treatment to address any changes promptly. Consulting healthcare providers if experiencing hearing-related changes is crucial for managing potential ototoxic effects of inhaled tobramycin.
What Antibiotics Cause Hearing Loss?
Absolutely, a notable fact is that various aminoglycoside antibiotics, including neomycin, kanamycin, amikacin, gentamicin, and tobramycin, can lead to hearing loss. Monitoring both medication levels and hearing function is essential when using these ototoxic antibiotics to prevent irreversible damage to the auditory system.
Genetic predispositions to aminoglycoside ototoxicity may necessitate closer monitoring with antibiotics like tobramycin to avert hearing impairment.
Conclusion
In conclusion, tobramycin's ototoxicity poses a significant risk to hearing health, damaging both vestibular and cochlear structures. By understanding the mechanisms of ototoxicity and implementing strategies for hair cell protection, healthcare providers can minimize the risk of irreversible hearing loss in patients undergoing treatment with aminoglycoside antibiotics.
Remember, when it comes to preserving hearing, prevention is key – as the saying goes, an ounce of prevention is worth a pound of cure.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Seizures Can Cause Hearing Loss: A Comprehensive Guide
Intriguing connections between seizures and hearing loss unveil surprising insights, hinting at a deeper relationship worth exploring further.

Exploring the intricate connection between seizures and hearing loss reveals a fascinating trend, highlighting the extent to which brain activity can impact more than expected.
The repercussions of seizures on auditory function reveal a complex interplay that warrants further investigation. Understanding how these neurological events can potentially lead to hearing impairment opens up a realm of possibilities in terms of treatment and management strategies.
The implications of this relationship are profound and offer a unique perspective on addressing the multifaceted nature of such conditions.
Key Takeaways
- Seizures damage auditory pathways, leading to temporary or permanent hearing loss.
- Abnormal neuronal excitability in epilepsy impacts inner ear function, causing sensorineural hearing impairment.
- Understanding mechanisms crucial for differentiating transient vs. long-term hearing issues post-seizures.
- Effective management strategies include personalized treatment, monitoring for side effects, and interdisciplinary collaboration.
Mechanisms of Seizure-Induced Hearing Loss
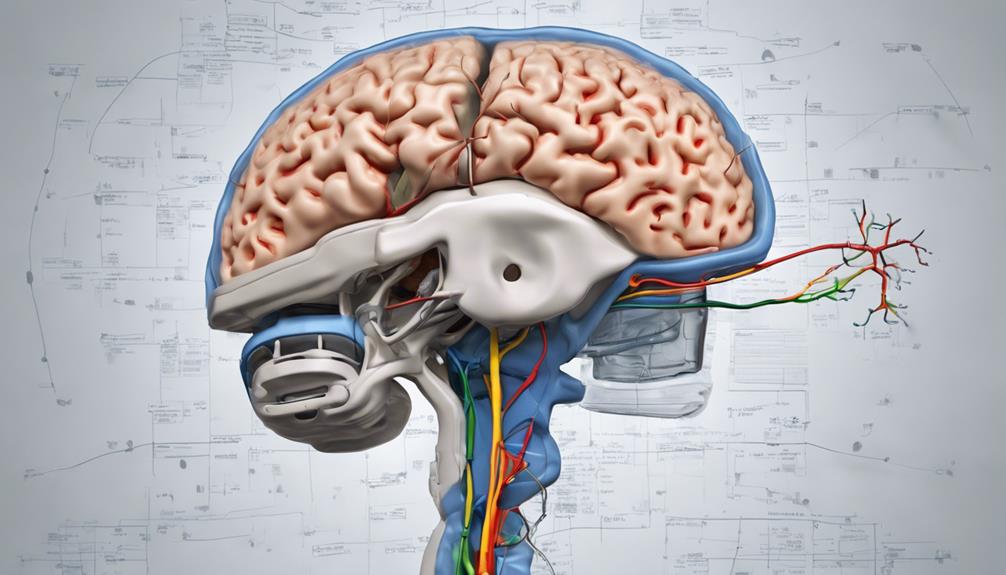
Seizures can directly damage the auditory pathways in the brain, leading to seizure-induced hearing loss. In individuals with epilepsy, abnormal neuronal excitability during focal seizures can impact the inner ear's function, resulting in sensorineural hearing loss. The disruption of auditory nerve pathways by seizure activity can cause temporary or permanent impairments in hearing. This process involves complex interactions between the electrical disturbances characteristic of seizures and the intricate mechanisms responsible for auditory signal transmission within the brain.
Furthermore, prolonged or severe seizures may trigger metabolic changes in the inner ear structures, affecting their ability to process sound effectively. These alterations can manifest as varying degrees of hearing loss, highlighting the importance of monitoring individuals with epilepsy for post-seizure auditory complications. Understanding the mechanisms underlying seizure-induced hearing loss is crucial for differentiating between transient hearing disturbances and potential long-term consequences on auditory health. By elucidating these intricate processes, healthcare professionals can better address the auditory challenges faced by individuals with epilepsy.
Types of Seizures Associated With Hearing Impairment

Among the various types of epileptic events, those affecting specific brain regions can lead to pronounced auditory symptoms, including hearing loss. Epilepsy with auditory features often involves seizures originating in the temporal lobe, impacting the auditory cortex and pathways crucial for hearing. Complex partial seizures with auditory manifestations such as buzzing, ringing, or abnormal sounds can disrupt normal hearing functions. Additionally, prolonged or severe seizures may result in damage to the auditory system, leading to post-seizure hearing loss.
| Types of Seizures Associated With Hearing Impairment | Description | Brain Regions Involved | Auditory Symptoms |
|---|---|---|---|
| Temporal Lobe Seizures | Arise in the temporal lobe | Temporal Lobe | Hearing loss, auditory hallucinations |
| Complex Partial Seizures with Auditory Features | Involve abnormal sounds perception | Auditory Cortex | Buzzing, ringing, abnormal auditory sensations |
| Seizures Causing Post-Seizure Hearing Loss | Result in hearing impairment post-seizure | Auditory Pathways | Temporary or permanent hearing loss |
Impact of Seizures on Auditory Pathways
Disruption of normal sound signal processing in the brain can occur as a result of seizures, potentially leading to temporary or permanent hearing loss. When seizures impact auditory pathways, they interfere with the intricate mechanisms involved in perceiving and interpreting sound.
Here are some key points to consider:
- Abnormal Electrical Activity: Seizures trigger abnormal electrical activity in the brain, disrupting the transmission of auditory signals.
- Temporary or Permanent Hearing Loss: Depending on the severity of the seizure and its effects on the auditory pathways, individuals may experience temporary or permanent hearing loss.
- Sensorineural Hearing Loss: Seizure-induced hearing loss often presents as sensorineural hearing loss, affecting the inner ear's ability to transmit sound effectively.
- Variability in Impact: The impact of seizures on auditory pathways can vary based on factors such as seizure type, duration, and intensity, highlighting the complex relationship between seizures and hearing complications.
Understanding how seizures affect auditory pathways is crucial for developing effective management strategies to mitigate the risk of associated hearing complications.
Treatment Approaches for Seizure-Related Hearing Loss

In the management of seizure-related hearing loss, the utilization of antiepileptic medications to control epilepsy plays a crucial role in minimizing the impact on auditory function. For individuals with an uncommon form of epilepsy that includes language before losing consciousness, such as focal impaired awareness seizures, antiepileptic drugs like carbamazepine and levetiracetam are commonly used. These medications help control seizures, potentially reducing the risk of hearing loss.
However, some individuals may not respond well to standard medications, necessitating personalized treatment strategies. Monitoring for potential side effects of antiepileptic drugs is essential in the management of seizure-related hearing loss, as these medications can have adverse effects on hearing and overall health. Collaboration between healthcare providers and specialists is crucial to develop a comprehensive treatment plan that addresses both the epilepsy and associated hearing issues effectively.
Managing Hearing Loss in Epilepsy Patients
When managing hearing loss in epilepsy patients, addressing the direct impact of seizures on the auditory system is paramount to understanding and addressing potential auditory impairments. Here are key considerations:
- Monitoring Post-Seizure Symptoms: Regularly assess for any changes in hearing after seizures to promptly identify and manage any emerging issues.
- Consulting Specialists: Seeking guidance from audiologists or otolaryngologists can aid in determining the extent of hearing loss and devising appropriate interventions.
- Investigating Underlying Causes: Explore potential factors such as medication side effects, neurological impacts of seizures, or genetic predispositions like autosomal dominant traits or family history of hearing loss.
- Managing Loss of Consciousness: Develop strategies to mitigate the risk of injury from falls during seizures, as head trauma can contribute to hearing impairment.
Frequently Asked Questions
Can Seizures Cause Hearing Loss?
Yes, seizures can cause hearing loss. The disruption of auditory processing in the brain during a seizure can lead to temporary hearing impairment. Post-seizure symptoms, such as hearing loss, are often reversible and may improve as the brain recovers.
Although the exact mechanism isn't fully understood, it's believed to involve transient changes in auditory function. Seeking timely medical evaluation and management can effectively address post-seizure hearing issues.
What Neurological Condition Causes Hearing Loss?
We explore the neurological condition causing hearing loss. Various factors, including autoimmune inner ear disease, Meniere's disease, or auditory neuropathy spectrum disorder, can lead to this impairment.
These conditions affect the auditory nerve or cochlea, disrupting sound transmission. Detailed evaluation and timely intervention are crucial to address such issues effectively.
Understanding the underlying neurological mechanisms is pivotal in managing and treating hearing loss associated with these conditions.
What Are the 4 Stages of a Seizure?
We understand the 4 stages of a seizure as follows: prodromal, aura, ictal, and postictal.
The prodromal phase shows early signs such as mood changes or headaches.
The aura stage involves sensory experiences like smells or sounds before the seizure.
The ictal phase is the seizure activity itself, characterized by convulsions or altered consciousness.
Does Your Brain Go Back to Normal After a Seizure?
After a seizure, the brain usually returns to its normal state during the postictal period. Our brain may go through temporary changes affecting cognitive and sensory functions, like hearing.
As the brain's electrical activity stabilizes, cognitive functions gradually recover, but some individuals may have lingering symptoms. Monitoring cognitive functions and addressing sensory issues post-seizure are crucial for optimal recovery.
Think of it like a storm passing, with the brain gradually returning to its calm state.
Conclusion
In conclusion, the intricate relationship between seizures and hearing loss highlights the importance of genetic analysis in diagnosing and managing auditory complications in epilepsy patients.
An interesting statistic to note is that up to 40% of individuals with epilepsy experience some form of hearing impairment, underscoring the need for comprehensive care strategies that address both neurological and auditory health concerns.
By understanding the molecular mechanisms at play, we can pave the way for personalized treatment approaches in the future.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Stroke Can Cause Hearing Loss in One Ear
Mysteries unravel as we delve into the intricate relationship between stroke and hearing loss in one ear, revealing unexpected connections.

When delving into the intricate connection between suffering a stroke and experiencing hearing loss in one ear, it is evident that the impact goes beyond just physical constraints. This correlation sheds light on the complex ways our bodies respond to these conditions.
Exploring how stroke can specifically lead to hearing loss in one ear unveils a fascinating yet crucial aspect of our overall well-being that warrants further exploration. The implications of this link extend far beyond what meets the eye, prompting a deeper examination into the mechanisms at play and the potential implications for holistic healthcare.
Key Takeaways
- Stroke-induced damage can lead to sudden sensorineural hearing loss in one ear.
- Ischemic strokes can significantly impact auditory pathways, affecting sound perception.
- Communication challenges and quality of life can be affected by hearing loss post-stroke.
- Early identification and management of hearing issues post-stroke are crucial for improved outcomes.
Stroke and Unilateral Hearing Loss
Stroke can lead to unilateral hearing loss, affecting one ear more significantly than the other due to disruptions in the auditory pathways caused by the brain damage. This hearing impairment can impact various aspects of auditory function, such as sound localization and speech understanding. The specific impact on hearing post-stroke can vary depending on the location and extent of the brain damage incurred during the stroke event. Individuals may struggle with accurately determining the direction of sounds or understanding speech in noisy environments due to this unilateral hearing loss.
Treatment options for unilateral hearing loss following a stroke may involve auditory rehabilitation programs aimed at improving speech comprehension and sound localization abilities. Additionally, the use of hearing aids can help individuals compensate for the hearing loss in the affected ear, enhancing their overall auditory experience and quality of life. Understanding the implications of stroke on hearing is crucial in developing effective interventions to address the impact of unilateral hearing loss in individuals who've experienced a stroke.
Mechanisms of Hearing Impairment Post-Stroke
Damage to the auditory pathways in the brain following a stroke can result in hearing impairment in one ear. The impact of stroke on hearing is multifaceted, with ischemic strokes and hemorrhagic strokes affecting auditory function through different mechanisms. Ischemic strokes, stemming from restricted blood flow, can disrupt the blood supply to specific auditory regions, leading to deficits in auditory processing. Conversely, hemorrhagic strokes, characterized by bleeding in the brain, may affect the auditory cortex and related structures, influencing how sound is perceived unilaterally. The location and extent of brain damage post-stroke play a crucial role in determining the nature and severity of hearing loss experienced in one ear. Understanding the intricate relationship between stroke and auditory pathways is essential for comprehensively addressing unilateral hearing impairments in stroke survivors.
| Mechanism | Type of Stroke | Effect on Hearing |
|---|---|---|
| Disrupted blood supply | Ischemic Stroke | Impacts specific auditory regions |
| Auditory cortex damage | Hemorrhagic Stroke | Affects auditory processing and perception |
Impact of Stroke on One Ear
Emerging research highlights the intricate relationship between auditory function and cerebral events, particularly emphasizing the impact of stroke on unilateral hearing abilities. When a stroke occurs, the disrupted blood supply can lead to damage in the auditory system of one ear. This damage affects the nerves and structures responsible for processing sound, potentially resulting in sudden sensorineural hearing loss in that ear. Ischemic strokes, which restrict blood flow to specific areas of the brain, can have a more pronounced impact on hearing in one ear compared to other types of strokes.
Monitoring changes in hearing in the affected ear post-stroke is crucial for the early detection and management of potential hearing loss. By closely monitoring the auditory function in stroke patients, healthcare providers can intervene promptly to mitigate the effects of hearing impairment. Understanding the relationship between strokes and hearing loss in one ear is essential for providing comprehensive care to individuals who've experienced a stroke.
Hearing Loss in Stroke Patients

Exploring the intricate relationship between stroke and auditory function reveals the significant impact of cerebrovascular events on hearing loss in patients. Hearing loss in stroke patients often stems from damage to the auditory pathways in the brain, particularly in cases where the stroke affects specific regions responsible for processing sound. This can result in sensorineural hearing loss, where the inner ear or the auditory nerve is impaired due to brain damage caused by the stroke. Communication difficulties may arise, impacting the quality of life for individuals experiencing this type of hearing loss.
The severity and manifestation of stroke-induced hearing loss can vary depending on the type and location of the stroke. Recognizing and managing hearing loss early on in stroke patients is crucial for effective rehabilitation and improved outcomes. By addressing hearing issues promptly, healthcare professionals can help minimize the negative impact on communication abilities and overall well-being. Early intervention and appropriate management strategies play a pivotal role in enhancing the quality of life for stroke survivors dealing with hearing loss.
Preventing Hearing Loss After Stroke
How can immediate medical interventions post-stroke contribute to preventing or minimizing hearing loss in affected individuals?
Monitoring for sudden changes in hearing post-stroke is essential, as prompt action can address emerging issues.
Rehabilitation therapies, including auditory training, play a crucial role in enhancing communication abilities post-stroke.
Healthcare providers recommend regular follow-ups to monitor and manage potential hearing loss effectively.
Prevention strategies post-stroke involve a multidisciplinary approach, including early identification of hearing issues and tailored interventions.
Comprehensive assessments by healthcare professionals can aid in early detection of hearing loss, leading to timely interventions.
Implementing personalized rehabilitation plans that incorporate auditory training can significantly improve outcomes for individuals at risk of hearing loss post-stroke.
Frequently Asked Questions
Why Did I Suddenly Lose My Hearing in One Ear?
We suddenly lost hearing in one ear due to various reasons like inner ear issues, infections, or even wax buildup.
It's essential to seek medical attention promptly to determine the underlying cause. Diagnostic tests can pinpoint the exact reason for the sudden hearing loss and guide appropriate treatment.
Monitoring any associated symptoms and following up with healthcare providers can aid in managing and potentially resolving the hearing loss.
What to Do When Can't Hear Out One Ear?
When we can't hear out of one ear, it's crucial to seek immediate medical attention. This sudden hearing loss could be a sign of various underlying conditions, including issues with the ear canal or inner ear.
Prompt evaluation by a healthcare professional can help diagnose the cause and determine the appropriate treatment. Ignoring unilateral hearing loss can lead to further complications, so it's essential to act swiftly and get the necessary medical care.
Can Hearing Loss From Stroke Be Reversed?
Yes, hearing loss from a stroke can sometimes be reversed through prompt medical intervention and targeted rehabilitation efforts. Immediate treatment for the underlying cause of the stroke is vital for improving the chances of reversing associated hearing loss.
Rehabilitation therapies like speech therapy and auditory training play a crucial role in restoring hearing function post-stroke. Factors such as the stroke's severity, affected brain area, and timely intervention influence the extent of recovery.
What Is the Most Common Cause of Unilateral Hearing Loss?
Damage to the inner ear or auditory nerve on one side is the most common cause of unilateral hearing loss. Other factors like infections, head trauma, acoustic neuroma, and Meniere's disease can also lead to hearing loss in one ear.
Unilateral hearing loss can impact sound localization, understanding speech in noisy environments, and overall quality of life. Seeking immediate medical attention is crucial when experiencing sudden or unexplained hearing loss in one ear to rule out serious underlying conditions.
Conclusion
In conclusion, the intricate relationship between stroke and hearing loss in one ear underscores the importance of maintaining cardiovascular health.
By understanding the mechanisms of auditory impairment post-stroke and recognizing the potential warning signs of sudden hearing loss, individuals can take proactive steps to prevent long-term consequences.
Just as blood vessels nourish both the brain and the ears, safeguarding against stroke risk factors can ultimately protect our precious sense of hearing.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
-
 Navigating the VA System4 weeks ago
Navigating the VA System4 weeks agoVA Hearing Loss Rating Chart: Understanding Disability Compensation
-

 Therapies and Interventions3 months ago
Therapies and Interventions3 months ago10 Auditory Processing Goals for Effective Speech Therapy
-

 Living with Hearing Loss2 months ago
Living with Hearing Loss2 months ago10 Deaf-Friendly Dating Sites to Find Your Perfect Match
-

 Sign Language3 months ago
Sign Language3 months agoSign Language Emoji Translator: How to Communicate With Gestures
-

 Tinnitus1 month ago
Tinnitus1 month agoVA's Rating System for Tinnitus and Hearing Loss Explained
-

 Navigating the VA System3 weeks ago
Navigating the VA System3 weeks agoUnderstanding Bilateral Hearing Loss VA Rating Criteria
-

 Vetted1 month ago
Vetted1 month ago15 Best Oticon Hearing Aids to Improve Your Hearing in 2024
-

 Living with Hearing Loss2 months ago
Living with Hearing Loss2 months agoAn Introduction to Deaf Culture: Understanding the Basics




















