While delving into the intricate connections and delicate ties of the brain, we uncover a situation where cerebral hemorrhages hinder our ability to comprehend the world around us.
The intricate relationship between these internal hemorrhages and the subtle symphony of sound remains a complex puzzle waiting to be unraveled.
Join us on a journey through the labyrinthine corridors of neuroscience as we decipher the silent whispers of how these silent intruders can disrupt the harmonious balance of hearing.
Key Takeaways
- Blood in inner ear disrupts sound transmission, impacting hearing post brain bleeds.
- Damage to temporal lobe affects auditory processing, leading to hearing difficulties.
- Impaired microcirculation in cochlea causes hearing loss after brain bleeds.
- Compression of auditory nerve interrupts signal transmission, contributing to auditory dysfunction.
Mechanisms of Hearing Loss Post Brain Bleeds
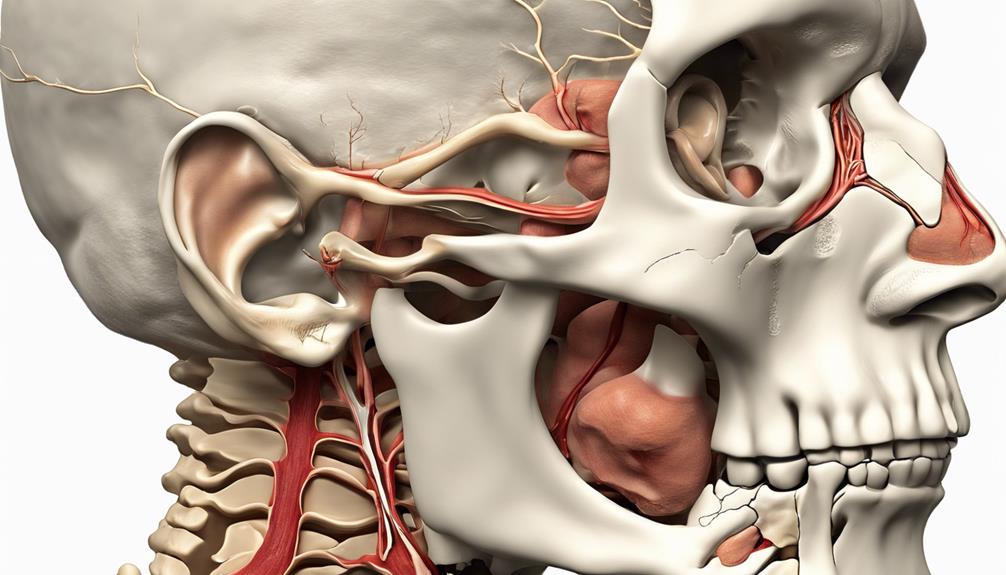
Blood in the inner ear resulting from brain bleeds directly disrupts the delicate structures responsible for sound transmission, leading to mechanisms of hearing loss post brain bleeds. One critical area affected by brain bleeds is the temporal lobe. Damage to this region can impact auditory processing and contribute to sensorineural hearing loss. The temporal lobe plays a crucial role in processing sound information and interpreting it for perception. When blood interferes with the functioning of this area, it can lead to difficulties in accurately perceiving and understanding sounds.
Moreover, sensorineural hearing loss can occur due to impaired microcirculation in the cochlea following brain bleeds. The reduced blood flow and oxygen supply to the cochlea can result in tissue damage, affecting the proper transmission of sound signals. Additionally, direct compression of the auditory nerve by brain bleeds can further exacerbate hearing impairment by interrupting the transmission of signals to the brain for interpretation. These intricate mechanisms highlight how brain bleeds can intricately disrupt the auditory system, leading to various forms of hearing loss.
Auditory Processing Deficits in Brain Bleeds

Continuing from the intricate mechanisms of hearing loss post brain bleeds, the impact of brain bleeds on auditory processing manifests through a range of deficits affecting the transmission of auditory signals from the inner ear to the auditory cortex.
Brain bleeds can disrupt the intricate neural pathways that relay auditory information, resulting in challenges in interpreting sounds correctly. The auditory cortex, a critical region responsible for processing sound signals, can be significantly affected by the damage caused by brain bleeds, leading to issues in recognizing and understanding auditory stimuli.
These deficits can manifest as difficulty in distinguishing speech sounds, locating the source of sounds, or comprehending complex auditory information. Understanding the specific alterations in auditory processing caused by brain bleeds is essential for diagnosing and addressing the associated hearing impairments effectively.
Peripheral Hearing Impairment Mechanisms
Exploring the mechanisms underlying peripheral hearing impairment post brain bleeds reveals intricate pathways and physiological changes that contribute to auditory dysfunction.
- Blood Flow Disturbances: Computed tomography scans often show evidence of blood leaking into the inner ear structures, disrupting their delicate function.
- Round Window Rupture: The rupture of the round window membrane due to increased pressure from hemorrhagic events can directly impact cochlear function, leading to hearing loss.
- Ischemic Cochlear Damage: Ischemia resulting from compromised blood flow to the cochlea can cause tissue damage, affecting the processing of auditory signals.
- Compression of Auditory Pathway: Hemorrhagic events can exert direct pressure on the auditory nerve, disrupting the transmission of signals along the auditory pathway.
Understanding these intricate mechanisms sheds light on the diverse ways in which brain bleeds can induce peripheral hearing impairment. By delving into the specifics of these processes, healthcare professionals can better comprehend the complexities of auditory dysfunction following such cerebrovascular events.
Clinical Implications for Hearing Loss

Upon examining the clinical implications of hearing loss following brain bleeds, it becomes evident that understanding the intricate relationship between intracerebral hemorrhage and auditory dysfunction is paramount for effective patient management. Hearing loss associated with brain bleeds can manifest suddenly and severely, particularly in cases of putaminal hemorrhage. This type of neurological cause should be considered in patients presenting with acute hearing impairment, as it may involve sensorineural hearing loss affecting both ears asymmetrically. The temporal relationship between the brain injury and the onset of hearing deficits is crucial for accurate diagnosis and timely intervention. Additionally, recognizing the potential for cortical hearing loss due to intracerebral hemorrhage underscores the necessity for a comprehensive evaluation and interdisciplinary approach to care.
| Clinical Implications for Hearing Loss | |
|---|---|
| Key Aspect | Significance |
| Relationship between brain bleeds and auditory dysfunction | Understanding temporal onset crucial |
| Types of hearing loss after brain injury | Sensorineural, asymmetric impact |
| Importance of comprehensive evaluation | Interdisciplinary care essential |
| Management considerations | Timely intervention critical |
Future Directions in Research
In our pursuit of advancing knowledge in the field, we aim to delve into novel imaging modalities that offer enhanced insights into the mechanisms underpinning post-brain bleed hearing loss. Future research endeavors will focus on the following aspects:
- Advanced Imaging Techniques: Developing cutting-edge imaging methods such as functional MRI or diffusion tensor imaging to visualize blood flow changes in auditory pathways post brain bleeds.
- Inflammation and Oxidative Stress: Investigating the impact of inflammation and oxidative stress on auditory processing following intracerebral hemorrhage to identify potential therapeutic targets.
- Long-Term Auditory Effects: Studying the prolonged effects of brain bleeds on auditory processing to optimize rehabilitation strategies for individuals with hearing impairment.
- Brain Region Connectivity: Exploring the intricate connections between hemorrhagic brain regions and auditory pathways to discover innovative interventions for restoring auditory function.
Frequently Asked Questions
Can a Brain Bleed Cause Hearing Loss?
Yes, a brain bleed can indeed cause hearing loss. Hemorrhages in the brain, such as intracerebral hemorrhage, can impact the auditory pathway, leading to sudden or unexplained hearing impairment. Regions like the putamen are particularly prone to causing sensorineural hearing loss.
It's crucial to consider neurological causes, like brain bleeds, when evaluating cases of hearing loss for proper management. Understanding this relationship is vital for effective treatment.
Can Brain Damage Cause Hearing Loss?
Yes, brain damage can cause hearing loss. When the brain sustains injury, like from a bleed, it can disrupt the auditory pathway. This disruption affects the brain's ability to process sound signals correctly, leading to hearing impairment.
Understanding this link between brain damage and hearing loss is crucial for prompt diagnosis and treatment. Early intervention can improve outcomes for individuals experiencing hearing difficulties due to brain injuries.
What Is the Most Feared Complication in Subarachnoid Hemorrhage?
Delayed cerebral ischemia is the most feared complication in subarachnoid hemorrhage. It occurs in around 30% of cases and can result in lasting neurological deficits. Factors like age, hypertension, smoking, aneurysm size, and other medical conditions increase the risk.
Timely detection and management are crucial to prevent further brain damage and complications like hearing loss. Vigilant monitoring for symptoms is vital in ensuring swift intervention and better patient outcomes.
What Are the 4 Types of Brain Bleeds?
We can categorize brain bleeds into four main types:
- Epidural bleeds occur between the skull and the dura mater from trauma.
- Subdural bleeds involve bleeding between the dura mater and the arachnoid mater due to trauma or vessel rupture.
- Subarachnoid bleeds happen in the subarachnoid space, typically due to aneurysm rupture.
- Intracerebral bleeds occur within brain tissue, causing symptoms like hearing loss.
Conclusion
As we delve into the intricate web of how brain bleeds can lead to hearing loss, we uncover a labyrinth of interconnected pathways and mechanisms. Like a delicate symphony disrupted by a sudden discordant note, the auditory system is vulnerable to the effects of intracerebral hemorrhage.
Through continued research and understanding, we can strive towards restoring harmony to the intricate dance of sound within the brain, offering hope for those grappling with the consequences of such neurological events.