Understanding Hearing Loss
How Mold Can Cause Hearing Loss: A Comprehensive Guide
Nestled in the overlooked realm of health hazards, the surprising link between mold and hearing loss awaits exploration.

Mold and hearing impairment might appear as an improbable pair, yet the influence of mold on our ear health is greater than we might anticipate. Ranging from fungal infections to respiratory complications that impact our hearing system, the link between exposure to mold and auditory issues is profound. Grasping the manner in which mold affects our hearing health is essential, with outcomes that can extend widely.
Let's explore the intricate relationship between mold and hearing loss, uncovering how this silent intruder can disrupt our hearing abilities without us even realizing it.
Key Takeaways
- Mold exposure can lead to fungal infections and respiratory issues affecting hearing.
- Certain types of mold, like Stachybotrys chartarum, can produce mycotoxins contributing to permanent hearing loss.
- Symptoms of mold-induced hearing impairment include muffled sounds, ear pain, and balance issues.
- Prevent mold-related hearing issues by ensuring proper ventilation, addressing leaks promptly, and keeping indoor spaces dry.
Types of Mold Linked to Hearing Loss
As experts in audiology research, we've identified several types of mold that are commonly associated with causing hearing loss. Mold species such as Aspergillus and Penicillium have been linked to ear infections and potential damage to hearing, especially in the middle ear where they can thrive.
The presence of Stachybotrys chartarum, commonly known as black mold, is concerning due to its production of mycotoxins which can contribute to permanent hearing loss. Additionally, molds like Alternaria and Cladosporium have been known to trigger allergic reactions leading to ear inflammation, potentially exacerbating existing conditions and impacting hearing abilities.
Furthermore, molds such as Fusarium and Trichoderma pose a risk of causing invasive fungal infections in the ear canal, which can result in severe consequences for hearing health. Exposure to these molds in indoor environments not only increases the likelihood of ear infections but also worsens any underlying issues, ultimately contributing to the development of hearing loss.
It's crucial to address mold exposure promptly to mitigate the risk of hearing impairment.
Symptoms of Mold-Induced Hearing Impairment

Signs of mold-induced hearing impairment encompass a range of symptoms that can manifest in various ways, indicating potential issues affecting auditory health. Loss of hearing due to mold exposure may present as muffled sounds, making it challenging to discern speech or other sounds clearly. Individuals experiencing mold-induced hearing damage might also notice ear pain, drainage, or discharge, which could be accompanied by recurring ear infections.
Distorted sounds and sensations of fullness in the ear can further suggest mold-related issues affecting hearing. Additionally, dizziness, balance problems, and changes in ear pressure are common symptoms of mold-induced hearing impairment. Itchy ears, redness, or swelling in the ear canal shouldn't be overlooked, as they could be indicative of underlying mold-related ear health issues.
Being aware of these signs and seeking prompt medical attention is crucial in addressing mold-induced hearing impairment effectively.
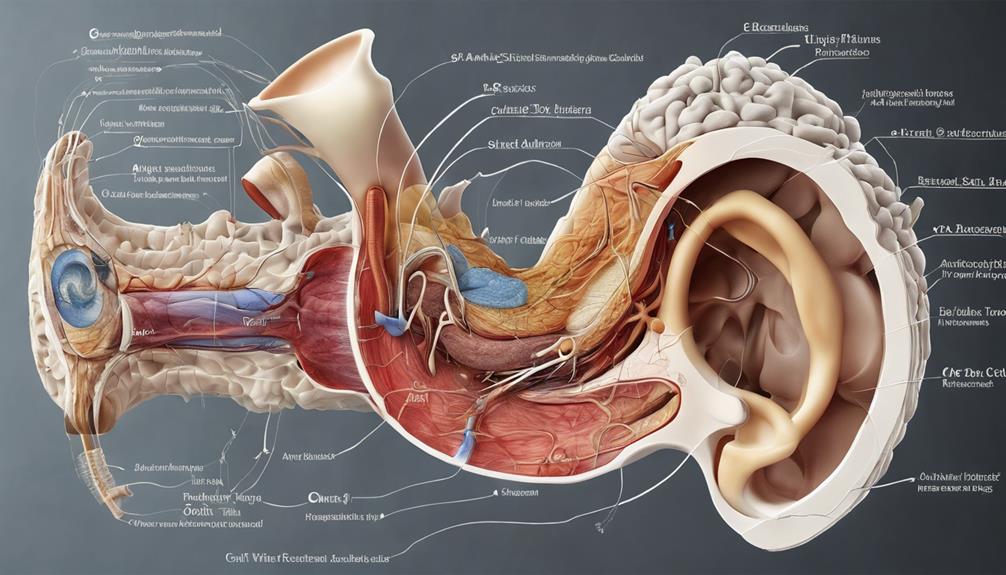
Impact of Mold on Ear Health
Exposure to mold can significantly impact ear health, potentially leading to fungal infections and respiratory issues that can detrimentally affect hearing. Mold spores, when inhaled, can cause fungal infections within the ear, directly affecting hearing health.
Additionally, respiratory infections triggered by mold exposure can harm the delicate structures of the ear, potentially resulting in hearing loss. Severe infections in the ear, sinus, or throat due to mold can disrupt the interconnectedness with the auditory system, leading to permanent hearing damage.
Changes in ear pressure resulting from mold-related infections can manifest as symptoms like tinnitus, characterized by buzzing or hissing sounds, commonly associated with hearing issues. If left untreated, severe ear infections caused by mold can escalate to eardrum rupture or permanent hearing loss, emphasizing the critical importance of addressing mold exposure promptly to safeguard ear health and prevent long-term auditory complications.
Preventing Mold-Related Hearing Issues

To mitigate the risk of mold-related hearing issues, implementing proper ventilation and moisture control measures in living spaces is crucial. Preventing mold growth through proactive strategies can significantly reduce the likelihood of developing mold-related ear infections. Here are some key steps to consider in maintaining a mold-free environment:
| Preventive Measures | Description | Benefits |
|---|---|---|
| Proper Ventilation | Ensure adequate airflow in all rooms. | Reduces moisture buildup, hindering mold growth. |
| Moisture Control | Address leaks and dampness promptly. | Prevents mold formation and potential ear issues. |
| Dehumidifiers Usage | Use in humid areas to lower moisture levels. | Inhibits mold growth, decreasing hearing risks. |
| Clean Indoor Spaces | Keep areas dry, especially bathrooms/kitchens. | Deters mold formation, reducing ear infection risks. |
Seeking Treatment for Mold-Associated Hearing Loss
When addressing mold-associated hearing loss, seeking timely medical intervention is paramount to prevent potential complications and ensure effective treatment. If you suspect mold-related hearing issues, it's crucial to seek medical attention promptly.
A healthcare provider might suggest antibiotics or antifungal medications to address fungal ear infections resulting from mold exposure, which can lead to hearing loss if left untreated. In some cases, a referral to an otolaryngologist or audiologist may be necessary for a specialized evaluation and treatment plan tailored to mold-associated hearing problems.
Specialists may recommend hearing aids or other assistive devices to manage permanent damage caused by mold exposure. Regular follow-up appointments with healthcare professionals are essential to monitor progress and ensure proper management of mold-induced hearing issues.
Frequently Asked Questions
Can Mold Exposure Cause Hearing Loss?
Yes, mold exposure can cause hearing loss. Fungal infections in the ear, respiratory infections affecting the ear, sinus, and throat, and severe ear, sinus, or throat infections all linked to mold exposure can impact hearing.
Furthermore, tinnitus, manifested by ear ringing, and changes in ear pressure from mold-related infections can contribute to hearing loss. In severe cases, eardrum rupture or permanent hearing damage may result from mold-related ear infections.
What Are the Symptoms of Mold Infection in the Brain?
When mold infects the brain, symptoms can vary widely, including headaches, dizziness, cognitive difficulties, confusion, memory loss, and changes in behavior. Other signs may include seizures, numbness, tingling sensations, blurred vision, light sensitivity, persistent fatigue, mood swings, and coordination problems.
These issues can indicate a serious problem that requires medical attention. Understanding the range of symptoms associated with mold infections in the brain is crucial for early detection and treatment.
What Are the Symptoms of Mold Exposure in Adults?
When exposed to mold, adults may present with symptoms like:
- Nasal congestion
- Coughing
- Skin rashes
Respiratory issues, fatigue, and heightened sensitivity to odors can also indicate mold exposure. Individuals with preexisting conditions, such as asthma, may experience worsened symptoms.
It's crucial to recognize signs like wheezing, shortness of breath, and persistent flu-like symptoms as potential indicators of mold exposure. Seeking medical advice promptly is essential for managing these symptoms.
What Are the Symptoms of Mold in the Gut?
When mold affects the gut, symptoms can manifest as abdominal pain, bloating, diarrhea, or constipation. Digestive issues like nausea, vomiting, fatigue, weight loss, and appetite changes may also occur.
The severity and type of symptoms can vary based on individual sensitivity, the specific mold involved, and the duration of exposure. Chronic exposure to mold in the gut can even lead to broader systemic health problems beyond just digestive disturbances.
Conclusion
In conclusion, mold exposure can significantly impact hearing health. Symptoms such as tinnitus and difficulty hearing are common indicators of mold-related hearing issues.
One interesting statistic to note is that fungal infections in the ear can occur in up to 25% of individuals exposed to mold. This highlights the importance of seeking medical attention and taking preventive measures to protect our ears from the harmful effects of mold.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Does Tobramycin Cause Hearing Loss? A Guide
Journey into the intricate connection between tobramycin and hearing loss to uncover the surprising ways it impacts our ears.
In terms of the impact of tobramycin on hearing loss, its importance may be underestimated.
Have you ever wondered how this common antibiotic can lead to potential damage in our ears?
Let's explore the intricate mechanisms behind tobramycin-induced hearing impairment and uncover the essential insights that can help us better understand and potentially mitigate this side effect.
Key Takeaways
- Tobramycin damages inner ear hair cells, leading to irreversible hearing loss.
- Genetic factors increase susceptibility to tobramycin-induced ototoxicity.
- Hair cell damage pathways involve disruption of essential cellular processes.
- Monitoring drug levels and genetic predispositions are crucial in preventing hearing loss.
Tobramycin's Mechanism of Ototoxicity
Tobramycin exerts its ototoxic effects by directly damaging the delicate hair cells within the inner ear, causing significant impairment in auditory function. This damage occurs primarily in the cochlea, a spiral-shaped structure responsible for converting sound vibrations into electrical signals that the brain can interpret. The inner ear houses sensory cells crucial for hearing, including the hair cells that detect sound waves and transmit signals to the auditory nerve. When tobramycin interferes with these hair cells, it can lead to permanent hearing loss.
The inner ear's intricate architecture makes it particularly vulnerable to the toxic effects of tobramycin. The drug disrupts the normal functioning of these hair cells, ultimately resulting in their degeneration and loss. Once these cells are damaged, they're unable to regenerate, leading to irreversible hearing impairment. This profound impact on the inner ear underscores the importance of monitoring tobramycin usage carefully, especially in individuals with genetic predispositions or mitochondrial DNA mutations that heighten susceptibility to ototoxicity.
Impact on Auditory Hair Cells
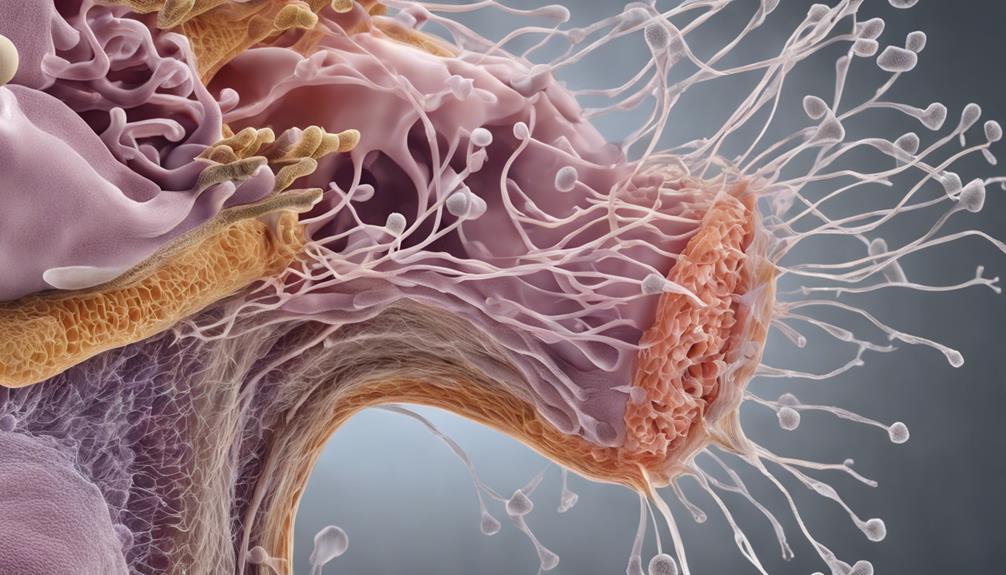
Damage to the delicate auditory hair cells in the inner ear is a critical consequence of tobramycin exposure, often resulting in irreversible hearing loss. Tobramycin, commonly used to treat infections like otitis media, exerts its ototoxic effects by directly damaging the sensory cells in the cochlea. This damage leads to sensorineural hearing loss, affecting the ability to perceive sound accurately. The side effects of tobramycin on auditory hair cells can have profound implications for individuals undergoing treatment with this medication, highlighting the importance of monitoring hearing function during therapy.
Understanding the specific pathways through which tobramycin impacts auditory hair cells is an active area of research. Researchers are working to elucidate the mechanisms involved in the toxicity of tobramycin to develop strategies that can mitigate or prevent hearing loss associated with its use. By unraveling the intricate processes through which tobramycin damages auditory hair cells, scientists aim to improve treatment outcomes and minimize the risk of irreversible hearing impairment for patients receiving this medication.
Genetic Factors in Hearing Loss
In understanding the potential genetic factors contributing to hearing loss, researchers have identified specific genetic markers and mitochondrial DNA mutations that can increase susceptibility to aminoglycoside-induced ototoxicity. Genetic susceptibility is a crucial aspect in the development of drug-induced hearing loss, particularly with ototoxic medications like tobramycin.
Here are key points to consider:
- Certain genetic factors and mitochondrial DNA mutations can predispose individuals to aminoglycoside ototoxicity, including hearing loss.
- Genetic susceptibility plays a significant role in drug-induced hearing loss associated with ototoxic medications like tobramycin.
- Patients with specific genetic predispositions require closer monitoring when using ototoxic medications to prevent hearing damage.
Mitochondrial DNA abnormalities are known to contribute to the risk of aminoglycoside-induced hearing loss. Avoiding ototoxic antibiotics in individuals with genetic susceptibility is essential to prevent permanent hearing impairment. Understanding these genetic factors is essential in personalized medicine approaches to mitigate the risk of ototoxicity and preserve hearing function.
Pathways of Ototoxic Hair Cell Damage

Among the mechanisms underlying ototoxic hair cell damage, a key pathway involves the disruption of crucial cellular processes essential for auditory function. Tobramycin, through its toxic effects on the cochlea, interferes with the maintenance of hair cell integrity and function. This disruption can lead to the degeneration and death of these sensory cells, resulting in sensorineural hearing loss.
The severity of tobramycin-induced hair cell damage can vary depending on factors such as dosage and duration of exposure. High-frequency hearing loss is a common manifestation of tobramycin ototoxicity, impacting the perception of sounds in the higher range. Both ears are typically affected by tobramycin-induced cochlear toxicity, contributing to bilateral hearing impairment.
Understanding the pathways through which tobramycin causes ototoxic hair cell damage is crucial in developing strategies to mitigate its severe side effects on hearing.
Strategies for Hair Cell Protection
Exploring proactive measures to safeguard hair cells from tobramycin-induced hearing impairment involves strategic considerations such as minimizing dosage, closely monitoring medication levels, and assessing genetic predispositions.
When aiming to protect hair cells from tobramycin's ototoxic effects, several key strategies can be implemented:
- Minimize Dosage: Utilize the lowest effective dosage of tobramycin to reduce the risk of ototoxicity and potential damage to hair cells.
- Monitor Medication Levels: Regularly monitor tobramycin levels, especially in individuals with compromised kidney function, to adjust dosages accordingly and mitigate ototoxic effects.
- Assess Genetic Predispositions: Consider genetic factors and mitochondrial DNA mutations that may predispose individuals to tobramycin-induced ototoxicity. Close monitoring is crucial in such cases to prevent irreversible damage to hair cells.
Frequently Asked Questions
Does Tobramycin Cause Hearing Loss?
Yes, tobramycin can cause hearing loss. It's important to monitor for signs like tinnitus, dizziness, and hearing impairment when taking this medication. Factors like dosage, treatment duration, and existing health conditions can increase the risk.
Genetic factors and mitochondrial DNA mutations may also play a role in susceptibility to tobramycin-induced ototoxicity. Being aware of these factors and closely monitoring for symptoms are crucial when using this antibiotic.
Can Tobramycin Eye Drops Cause Ototoxicity?
Yes, tobramycin eye drops can cause ototoxicity, leading to hearing loss. While the risk is lower than with systemic use, it's still a concern.
Symptoms may include hearing loss, tinnitus, and balance issues. Following prescribed usage and promptly reporting any unusual symptoms to a healthcare provider is crucial for preventing ototoxicity.
It's essential to be vigilant and proactive in monitoring for these potential side effects.
Can You Get Ototoxicity From Inhaled Tobramycin?
Yes, ototoxicity can occur from inhaled tobramycin, potentially resulting in hearing loss and balance issues. However, the risk is generally lower when compared to systemic administration.
It's vital to monitor for any signs of hearing impairment while undergoing inhaled tobramycin treatment to address any changes promptly. Consulting healthcare providers if experiencing hearing-related changes is crucial for managing potential ototoxic effects of inhaled tobramycin.
What Antibiotics Cause Hearing Loss?
Absolutely, a notable fact is that various aminoglycoside antibiotics, including neomycin, kanamycin, amikacin, gentamicin, and tobramycin, can lead to hearing loss. Monitoring both medication levels and hearing function is essential when using these ototoxic antibiotics to prevent irreversible damage to the auditory system.
Genetic predispositions to aminoglycoside ototoxicity may necessitate closer monitoring with antibiotics like tobramycin to avert hearing impairment.
Conclusion
In conclusion, tobramycin's ototoxicity poses a significant risk to hearing health, damaging both vestibular and cochlear structures. By understanding the mechanisms of ototoxicity and implementing strategies for hair cell protection, healthcare providers can minimize the risk of irreversible hearing loss in patients undergoing treatment with aminoglycoside antibiotics.
Remember, when it comes to preserving hearing, prevention is key – as the saying goes, an ounce of prevention is worth a pound of cure.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Seizures Can Cause Hearing Loss: A Comprehensive Guide
Intriguing connections between seizures and hearing loss unveil surprising insights, hinting at a deeper relationship worth exploring further.

Exploring the intricate connection between seizures and hearing loss reveals a fascinating trend, highlighting the extent to which brain activity can impact more than expected.
The repercussions of seizures on auditory function reveal a complex interplay that warrants further investigation. Understanding how these neurological events can potentially lead to hearing impairment opens up a realm of possibilities in terms of treatment and management strategies.
The implications of this relationship are profound and offer a unique perspective on addressing the multifaceted nature of such conditions.
Key Takeaways
- Seizures damage auditory pathways, leading to temporary or permanent hearing loss.
- Abnormal neuronal excitability in epilepsy impacts inner ear function, causing sensorineural hearing impairment.
- Understanding mechanisms crucial for differentiating transient vs. long-term hearing issues post-seizures.
- Effective management strategies include personalized treatment, monitoring for side effects, and interdisciplinary collaboration.
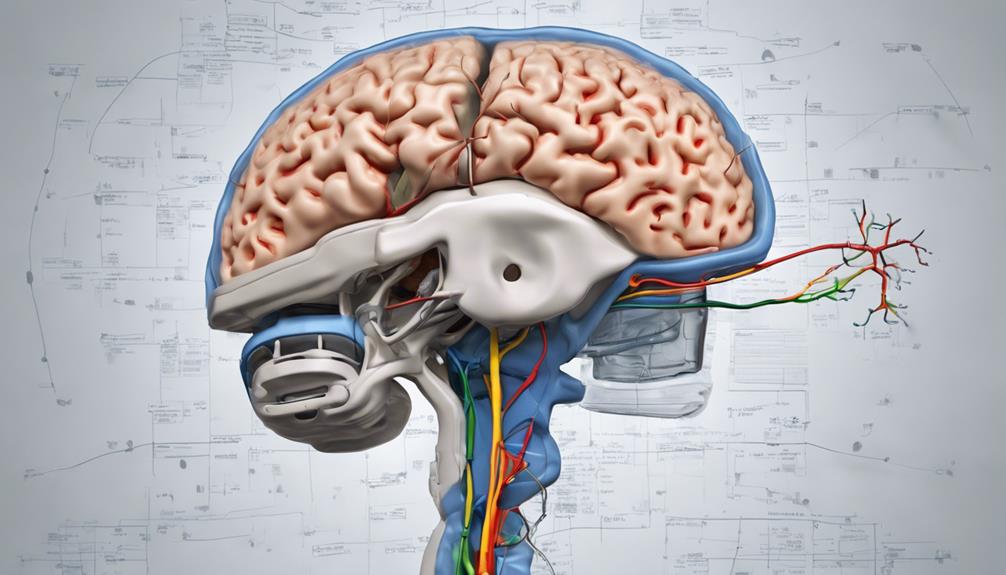
Mechanisms of Seizure-Induced Hearing Loss
Seizures can directly damage the auditory pathways in the brain, leading to seizure-induced hearing loss. In individuals with epilepsy, abnormal neuronal excitability during focal seizures can impact the inner ear's function, resulting in sensorineural hearing loss. The disruption of auditory nerve pathways by seizure activity can cause temporary or permanent impairments in hearing. This process involves complex interactions between the electrical disturbances characteristic of seizures and the intricate mechanisms responsible for auditory signal transmission within the brain.
Furthermore, prolonged or severe seizures may trigger metabolic changes in the inner ear structures, affecting their ability to process sound effectively. These alterations can manifest as varying degrees of hearing loss, highlighting the importance of monitoring individuals with epilepsy for post-seizure auditory complications. Understanding the mechanisms underlying seizure-induced hearing loss is crucial for differentiating between transient hearing disturbances and potential long-term consequences on auditory health. By elucidating these intricate processes, healthcare professionals can better address the auditory challenges faced by individuals with epilepsy.
Types of Seizures Associated With Hearing Impairment

Among the various types of epileptic events, those affecting specific brain regions can lead to pronounced auditory symptoms, including hearing loss. Epilepsy with auditory features often involves seizures originating in the temporal lobe, impacting the auditory cortex and pathways crucial for hearing. Complex partial seizures with auditory manifestations such as buzzing, ringing, or abnormal sounds can disrupt normal hearing functions. Additionally, prolonged or severe seizures may result in damage to the auditory system, leading to post-seizure hearing loss.
| Types of Seizures Associated With Hearing Impairment | Description | Brain Regions Involved | Auditory Symptoms |
|---|---|---|---|
| Temporal Lobe Seizures | Arise in the temporal lobe | Temporal Lobe | Hearing loss, auditory hallucinations |
| Complex Partial Seizures with Auditory Features | Involve abnormal sounds perception | Auditory Cortex | Buzzing, ringing, abnormal auditory sensations |
| Seizures Causing Post-Seizure Hearing Loss | Result in hearing impairment post-seizure | Auditory Pathways | Temporary or permanent hearing loss |
Impact of Seizures on Auditory Pathways
Disruption of normal sound signal processing in the brain can occur as a result of seizures, potentially leading to temporary or permanent hearing loss. When seizures impact auditory pathways, they interfere with the intricate mechanisms involved in perceiving and interpreting sound.
Here are some key points to consider:
- Abnormal Electrical Activity: Seizures trigger abnormal electrical activity in the brain, disrupting the transmission of auditory signals.
- Temporary or Permanent Hearing Loss: Depending on the severity of the seizure and its effects on the auditory pathways, individuals may experience temporary or permanent hearing loss.
- Sensorineural Hearing Loss: Seizure-induced hearing loss often presents as sensorineural hearing loss, affecting the inner ear's ability to transmit sound effectively.
- Variability in Impact: The impact of seizures on auditory pathways can vary based on factors such as seizure type, duration, and intensity, highlighting the complex relationship between seizures and hearing complications.
Understanding how seizures affect auditory pathways is crucial for developing effective management strategies to mitigate the risk of associated hearing complications.
Treatment Approaches for Seizure-Related Hearing Loss

In the management of seizure-related hearing loss, the utilization of antiepileptic medications to control epilepsy plays a crucial role in minimizing the impact on auditory function. For individuals with an uncommon form of epilepsy that includes language before losing consciousness, such as focal impaired awareness seizures, antiepileptic drugs like carbamazepine and levetiracetam are commonly used. These medications help control seizures, potentially reducing the risk of hearing loss.
However, some individuals may not respond well to standard medications, necessitating personalized treatment strategies. Monitoring for potential side effects of antiepileptic drugs is essential in the management of seizure-related hearing loss, as these medications can have adverse effects on hearing and overall health. Collaboration between healthcare providers and specialists is crucial to develop a comprehensive treatment plan that addresses both the epilepsy and associated hearing issues effectively.
Managing Hearing Loss in Epilepsy Patients
When managing hearing loss in epilepsy patients, addressing the direct impact of seizures on the auditory system is paramount to understanding and addressing potential auditory impairments. Here are key considerations:
- Monitoring Post-Seizure Symptoms: Regularly assess for any changes in hearing after seizures to promptly identify and manage any emerging issues.
- Consulting Specialists: Seeking guidance from audiologists or otolaryngologists can aid in determining the extent of hearing loss and devising appropriate interventions.
- Investigating Underlying Causes: Explore potential factors such as medication side effects, neurological impacts of seizures, or genetic predispositions like autosomal dominant traits or family history of hearing loss.
- Managing Loss of Consciousness: Develop strategies to mitigate the risk of injury from falls during seizures, as head trauma can contribute to hearing impairment.
Frequently Asked Questions
Can Seizures Cause Hearing Loss?
Yes, seizures can cause hearing loss. The disruption of auditory processing in the brain during a seizure can lead to temporary hearing impairment. Post-seizure symptoms, such as hearing loss, are often reversible and may improve as the brain recovers.
Although the exact mechanism isn't fully understood, it's believed to involve transient changes in auditory function. Seeking timely medical evaluation and management can effectively address post-seizure hearing issues.
What Neurological Condition Causes Hearing Loss?
We explore the neurological condition causing hearing loss. Various factors, including autoimmune inner ear disease, Meniere's disease, or auditory neuropathy spectrum disorder, can lead to this impairment.
These conditions affect the auditory nerve or cochlea, disrupting sound transmission. Detailed evaluation and timely intervention are crucial to address such issues effectively.
Understanding the underlying neurological mechanisms is pivotal in managing and treating hearing loss associated with these conditions.
What Are the 4 Stages of a Seizure?
We understand the 4 stages of a seizure as follows: prodromal, aura, ictal, and postictal.
The prodromal phase shows early signs such as mood changes or headaches.
The aura stage involves sensory experiences like smells or sounds before the seizure.
The ictal phase is the seizure activity itself, characterized by convulsions or altered consciousness.
Does Your Brain Go Back to Normal After a Seizure?
After a seizure, the brain usually returns to its normal state during the postictal period. Our brain may go through temporary changes affecting cognitive and sensory functions, like hearing.
As the brain's electrical activity stabilizes, cognitive functions gradually recover, but some individuals may have lingering symptoms. Monitoring cognitive functions and addressing sensory issues post-seizure are crucial for optimal recovery.
Think of it like a storm passing, with the brain gradually returning to its calm state.
Conclusion
In conclusion, the intricate relationship between seizures and hearing loss highlights the importance of genetic analysis in diagnosing and managing auditory complications in epilepsy patients.
An interesting statistic to note is that up to 40% of individuals with epilepsy experience some form of hearing impairment, underscoring the need for comprehensive care strategies that address both neurological and auditory health concerns.
By understanding the molecular mechanisms at play, we can pave the way for personalized treatment approaches in the future.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
Understanding Hearing Loss
How Stroke Can Cause Hearing Loss in One Ear
Mysteries unravel as we delve into the intricate relationship between stroke and hearing loss in one ear, revealing unexpected connections.

When delving into the intricate connection between suffering a stroke and experiencing hearing loss in one ear, it is evident that the impact goes beyond just physical constraints. This correlation sheds light on the complex ways our bodies respond to these conditions.
Exploring how stroke can specifically lead to hearing loss in one ear unveils a fascinating yet crucial aspect of our overall well-being that warrants further exploration. The implications of this link extend far beyond what meets the eye, prompting a deeper examination into the mechanisms at play and the potential implications for holistic healthcare.
Key Takeaways
- Stroke-induced damage can lead to sudden sensorineural hearing loss in one ear.
- Ischemic strokes can significantly impact auditory pathways, affecting sound perception.
- Communication challenges and quality of life can be affected by hearing loss post-stroke.
- Early identification and management of hearing issues post-stroke are crucial for improved outcomes.
Stroke and Unilateral Hearing Loss
Stroke can lead to unilateral hearing loss, affecting one ear more significantly than the other due to disruptions in the auditory pathways caused by the brain damage. This hearing impairment can impact various aspects of auditory function, such as sound localization and speech understanding. The specific impact on hearing post-stroke can vary depending on the location and extent of the brain damage incurred during the stroke event. Individuals may struggle with accurately determining the direction of sounds or understanding speech in noisy environments due to this unilateral hearing loss.
Treatment options for unilateral hearing loss following a stroke may involve auditory rehabilitation programs aimed at improving speech comprehension and sound localization abilities. Additionally, the use of hearing aids can help individuals compensate for the hearing loss in the affected ear, enhancing their overall auditory experience and quality of life. Understanding the implications of stroke on hearing is crucial in developing effective interventions to address the impact of unilateral hearing loss in individuals who've experienced a stroke.
Mechanisms of Hearing Impairment Post-Stroke
Damage to the auditory pathways in the brain following a stroke can result in hearing impairment in one ear. The impact of stroke on hearing is multifaceted, with ischemic strokes and hemorrhagic strokes affecting auditory function through different mechanisms. Ischemic strokes, stemming from restricted blood flow, can disrupt the blood supply to specific auditory regions, leading to deficits in auditory processing. Conversely, hemorrhagic strokes, characterized by bleeding in the brain, may affect the auditory cortex and related structures, influencing how sound is perceived unilaterally. The location and extent of brain damage post-stroke play a crucial role in determining the nature and severity of hearing loss experienced in one ear. Understanding the intricate relationship between stroke and auditory pathways is essential for comprehensively addressing unilateral hearing impairments in stroke survivors.
| Mechanism | Type of Stroke | Effect on Hearing |
|---|---|---|
| Disrupted blood supply | Ischemic Stroke | Impacts specific auditory regions |
| Auditory cortex damage | Hemorrhagic Stroke | Affects auditory processing and perception |
Impact of Stroke on One Ear
Emerging research highlights the intricate relationship between auditory function and cerebral events, particularly emphasizing the impact of stroke on unilateral hearing abilities. When a stroke occurs, the disrupted blood supply can lead to damage in the auditory system of one ear. This damage affects the nerves and structures responsible for processing sound, potentially resulting in sudden sensorineural hearing loss in that ear. Ischemic strokes, which restrict blood flow to specific areas of the brain, can have a more pronounced impact on hearing in one ear compared to other types of strokes.
Monitoring changes in hearing in the affected ear post-stroke is crucial for the early detection and management of potential hearing loss. By closely monitoring the auditory function in stroke patients, healthcare providers can intervene promptly to mitigate the effects of hearing impairment. Understanding the relationship between strokes and hearing loss in one ear is essential for providing comprehensive care to individuals who've experienced a stroke.
Hearing Loss in Stroke Patients

Exploring the intricate relationship between stroke and auditory function reveals the significant impact of cerebrovascular events on hearing loss in patients. Hearing loss in stroke patients often stems from damage to the auditory pathways in the brain, particularly in cases where the stroke affects specific regions responsible for processing sound. This can result in sensorineural hearing loss, where the inner ear or the auditory nerve is impaired due to brain damage caused by the stroke. Communication difficulties may arise, impacting the quality of life for individuals experiencing this type of hearing loss.
The severity and manifestation of stroke-induced hearing loss can vary depending on the type and location of the stroke. Recognizing and managing hearing loss early on in stroke patients is crucial for effective rehabilitation and improved outcomes. By addressing hearing issues promptly, healthcare professionals can help minimize the negative impact on communication abilities and overall well-being. Early intervention and appropriate management strategies play a pivotal role in enhancing the quality of life for stroke survivors dealing with hearing loss.
Preventing Hearing Loss After Stroke
How can immediate medical interventions post-stroke contribute to preventing or minimizing hearing loss in affected individuals?
Monitoring for sudden changes in hearing post-stroke is essential, as prompt action can address emerging issues.
Rehabilitation therapies, including auditory training, play a crucial role in enhancing communication abilities post-stroke.
Healthcare providers recommend regular follow-ups to monitor and manage potential hearing loss effectively.
Prevention strategies post-stroke involve a multidisciplinary approach, including early identification of hearing issues and tailored interventions.
Comprehensive assessments by healthcare professionals can aid in early detection of hearing loss, leading to timely interventions.
Implementing personalized rehabilitation plans that incorporate auditory training can significantly improve outcomes for individuals at risk of hearing loss post-stroke.
Frequently Asked Questions
Why Did I Suddenly Lose My Hearing in One Ear?
We suddenly lost hearing in one ear due to various reasons like inner ear issues, infections, or even wax buildup.
It's essential to seek medical attention promptly to determine the underlying cause. Diagnostic tests can pinpoint the exact reason for the sudden hearing loss and guide appropriate treatment.
Monitoring any associated symptoms and following up with healthcare providers can aid in managing and potentially resolving the hearing loss.
What to Do When Can't Hear Out One Ear?
When we can't hear out of one ear, it's crucial to seek immediate medical attention. This sudden hearing loss could be a sign of various underlying conditions, including issues with the ear canal or inner ear.
Prompt evaluation by a healthcare professional can help diagnose the cause and determine the appropriate treatment. Ignoring unilateral hearing loss can lead to further complications, so it's essential to act swiftly and get the necessary medical care.
Can Hearing Loss From Stroke Be Reversed?
Yes, hearing loss from a stroke can sometimes be reversed through prompt medical intervention and targeted rehabilitation efforts. Immediate treatment for the underlying cause of the stroke is vital for improving the chances of reversing associated hearing loss.
Rehabilitation therapies like speech therapy and auditory training play a crucial role in restoring hearing function post-stroke. Factors such as the stroke's severity, affected brain area, and timely intervention influence the extent of recovery.
What Is the Most Common Cause of Unilateral Hearing Loss?
Damage to the inner ear or auditory nerve on one side is the most common cause of unilateral hearing loss. Other factors like infections, head trauma, acoustic neuroma, and Meniere's disease can also lead to hearing loss in one ear.
Unilateral hearing loss can impact sound localization, understanding speech in noisy environments, and overall quality of life. Seeking immediate medical attention is crucial when experiencing sudden or unexplained hearing loss in one ear to rule out serious underlying conditions.
Conclusion
In conclusion, the intricate relationship between stroke and hearing loss in one ear underscores the importance of maintaining cardiovascular health.
By understanding the mechanisms of auditory impairment post-stroke and recognizing the potential warning signs of sudden hearing loss, individuals can take proactive steps to prevent long-term consequences.
Just as blood vessels nourish both the brain and the ears, safeguarding against stroke risk factors can ultimately protect our precious sense of hearing.
Taylor brings a dynamic and analytical perspective to the Deaf Vibes team, focusing on research-driven content that educates and informs. With an unquenchable curiosity for new developments, policies, and social issues affecting the deaf and hard-of-hearing community, Taylor’s writing is a crucial resource for readers seeking to navigate these areas. Whether breaking down legal rights, highlighting educational opportunities, or offering guides on accessible technology, Taylor’s work is an invaluable asset to those seeking to empower themselves and others. Taylor’s commitment to accuracy and depth ensures that our readers have access to reliable and actionable information.
-
 Navigating the VA System4 weeks ago
Navigating the VA System4 weeks agoVA Hearing Loss Rating Chart: Understanding Disability Compensation
-

 Therapies and Interventions3 months ago
Therapies and Interventions3 months ago10 Auditory Processing Goals for Effective Speech Therapy
-

 Living with Hearing Loss2 months ago
Living with Hearing Loss2 months ago10 Deaf-Friendly Dating Sites to Find Your Perfect Match
-

 Sign Language3 months ago
Sign Language3 months agoSign Language Emoji Translator: How to Communicate With Gestures
-

 Tinnitus1 month ago
Tinnitus1 month agoVA's Rating System for Tinnitus and Hearing Loss Explained
-

 Navigating the VA System3 weeks ago
Navigating the VA System3 weeks agoUnderstanding Bilateral Hearing Loss VA Rating Criteria
-

 Vetted1 month ago
Vetted1 month ago15 Best Oticon Hearing Aids to Improve Your Hearing in 2024
-

 Living with Hearing Loss2 months ago
Living with Hearing Loss2 months agoAn Introduction to Deaf Culture: Understanding the Basics