Imagine a gentle melody echoing through the intricate passageways of your ears, with each note playing a vital role in your hearing.
Now, consider how Rheumatoid Arthritis, a condition often associated with joint pain, can quietly orchestrate a symphony of effects that extend beyond the bones and joints.
As we unravel the connection between RA and hearing loss, we uncover a complex interplay that challenges conventional perceptions of this autoimmune disease.
Stay tuned as we navigate the intricate mechanisms through which RA can influence our ability to perceive sound, prompting a deeper exploration of the nuances within this perplexing relationship.
Key Takeaways
- Sensorineural hearing loss is common in RA, impacting 75% of patients.
- RA-related inflammation damages inner ear structures, leading to hearing impairment.
- Medications like NSAIDs and antibiotics can exacerbate hearing issues in RA.
- Early detection through audiometric tests and collaborative care is crucial for managing RA-related hearing loss.

Audien Atom One OTC Hearing Aids – Wireless, Rechargeable, and Comfortable | Clear Sound in a Small, Discreet Design for Seniors & Adults with Hearing Loss
Hear What Matters Most: Hearing isn’t one-size-fits-all. That’s why our adjustable frequency system lets you personalize your sound…
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Types of Hearing Loss in RA
Sensorineural hearing loss is the most prevalent type of hearing impairment experienced by individuals with rheumatoid arthritis (RA). Unlike conductive hearing loss, which occurs due to problems in the outer or middle ear, sensorineural hearing loss in RA affects the inner ear or the auditory nerve pathways to the brain. RA patients are more likely to develop sensorineural hearing loss compared to the general population. Symptoms can manifest as muffled hearing, difficulty understanding speech, or ringing in the ear.
Less common types of hearing loss in RA include conductive and mixed hearing loss, which may involve both sensorineural and conductive components. Understanding the types of hearing loss that can occur in RA is crucial for early detection and appropriate treatment. By recognizing the specific challenges associated with different types of hearing loss in RA, healthcare providers can offer tailored interventions such as steroids, hearing aids, or surgery to improve the quality of life for affected individuals.
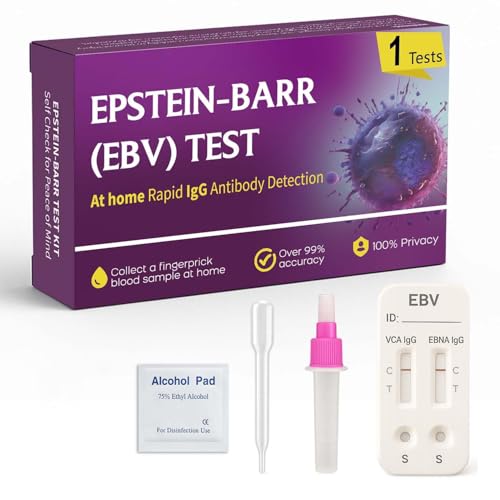
EBV at-Home Test Kit | Detects IgG Response to VCA & EBNA | 15-Minute Rapid Result | Easy Fingerstick Sample
Quick At-Home Screening – Designed for personal use, this test provides insight into your body’s immune response to…
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Link Between RA and Hearing Problems
The connection between rheumatoid arthritis (RA) and hearing problems underscores the intricate relationship between autoimmune conditions and auditory health. Individuals with RA face a heightened risk of hearing impairment, particularly sensorineural hearing loss, affecting around 75% of RA patients. This impairment stems from autoimmune inner ear disease (AIED), where inflammatory processes damage inner ear structures, including cochlear hair cells crucial for hearing. Moreover, RA treatment involving ototoxic drugs like methotrexate and hydroxychloroquine can exacerbate hearing issues.
To address these challenges, early detection through regular audiometric tests is essential. Treatment options for hearing problems in RA patients often include therapies such as steroids and immune system drugs to manage AIED and prevent further deterioration. Understanding the link between RA and hearing impairment empowers individuals to prioritize their auditory health alongside managing their autoimmune condition effectively.
- RA patients have a higher risk of sensorineural hearing loss.
- Autoimmune inner ear disease (AIED) can lead to hearing loss in RA patients.
- Inflammatory processes in RA can damage inner ear structures.
- RA treatment drugs like methotrexate and hydroxychloroquine can have ototoxic effects.

Vanderfields Premium Hearing Protection Ear Muffs – Broad Spectrum Sound Reduction 33.2dB at 2K Hz Noise Cancelling – Headset Safety Noise Cancellation – Headphones Adults and Teens – Marine Blue
SUPERIOR SOUND REDUCTION – Patented globally recognized design; Individually tested across the entire hearing spectrum; Certified 26 dB…
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Medication Risks for Hearing in RA
Regularly monitoring medication usage and discussing potential ototoxic effects with healthcare providers is crucial for managing hearing health in individuals with rheumatoid arthritis (RA).
Certain medications commonly used in RA treatment, such as NSAIDs, aspirin, and acetaminophen, have been linked to an increased risk of hearing loss in RA patients. Men under 60 who use these drugs frequently are particularly vulnerable to hearing issues related to RA, while women under 50 using acetaminophen or ibuprofen more regularly also face an elevated risk.
In addition to these pain relievers, antibiotics, chemotherapy drugs, and diuretics are examples of medications that can have ototoxic effects and impact hearing in RA patients.
Understanding the potential risks associated with these medications and having open discussions with healthcare providers can help individuals make informed decisions about their treatment plans and take proactive steps to preserve their hearing health while managing RA effectively.

Phonak Hearing Aid Drying Capsules
Phonak Hearing Aid Clean & Care Line Drying Capsules
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Early Detection of Hearing Loss in RA Patients

Detecting early signs of hearing loss in individuals with rheumatoid arthritis is crucial for timely intervention and effective management of their auditory health. Collaborative efforts between rheumatologists and audiologists play a vital role in achieving timely diagnosis and appropriate management strategies for RA patients experiencing hearing loss.
To aid in the early detection of hearing impairment in RA patients, several key assessments can be utilized:
- Pure Tone Audiometry (PTA): This comprehensive test helps identify the thresholds of hearing sensitivity across different frequencies, enabling early detection of any hearing loss.
- Extended High-Frequency Audiometry (EHFA): EHFA is particularly useful in detecting high-frequency hearing loss, which is common in RA patients and may go unnoticed without specific testing.
- Otoacoustic Emissions (OAEs): Absent OAEs can indicate early cochlear hearing loss, underscoring the importance of regular screenings for RA patients.
- Regular Screenings: Routine audiometric tests, including high-frequency audiometry, are essential for the early identification and monitoring of arthritis-related hearing loss in RA patients.
Management Strategies for RA-Related Hearing Loss
Collaborating closely with both rheumatologists and audiologists, we implement tailored management strategies to address hearing loss associated with rheumatoid arthritis, focusing on regular monitoring and potential adjustments in treatment plans. Audiometric tests play a crucial role in tracking changes in hearing function over time, guiding the management of RA-related hearing loss. When necessary, adjustments in RA medications are considered to prevent further damage to the auditory system. This collaborative approach ensures that patients receive comprehensive care that addresses both their rheumatoid arthritis and associated hearing issues.
In cases where cochlear hearing loss is detected early, prompt intervention is essential to explore the possibility of cochlear implants for severe hearing impairments. By taking preventive measures such as avoiding exposure to damaging noise sources, individuals with RA can reduce the risk of developing hearing loss. The partnership between rheumatologists and audiologists is key in developing effective management strategies that improve the quality of life for RA patients experiencing hearing difficulties.
Frequently Asked Questions
What Is the Life Expectancy of a Person With Rheumatoid Arthritis?
We know that the life expectancy of a person with rheumatoid arthritis can be affected by various factors such as disease activity, severity, comorbidities, and treatment response. Early diagnosis, aggressive treatment, and managing cardiovascular risks are crucial for improving outcomes.
Studies show that well-controlled disease can lead to a life expectancy closer to the general population. Monitoring, medication adherence, healthy choices, and quality healthcare access are key for optimizing outcomes.
What Are the 4 Stages of Rheumatoid Arthritis?
In rheumatoid arthritis, the 4 stages progress from early joint pain and stiffness in Stage 1 to severe joint destruction in Stage 3 and extensive damage in Stage 4.
Each stage brings increased challenges like deformities, disability, and systemic complications.
Understanding these stages helps us grasp the disease's severity and plan appropriate management strategies for improved quality of life.
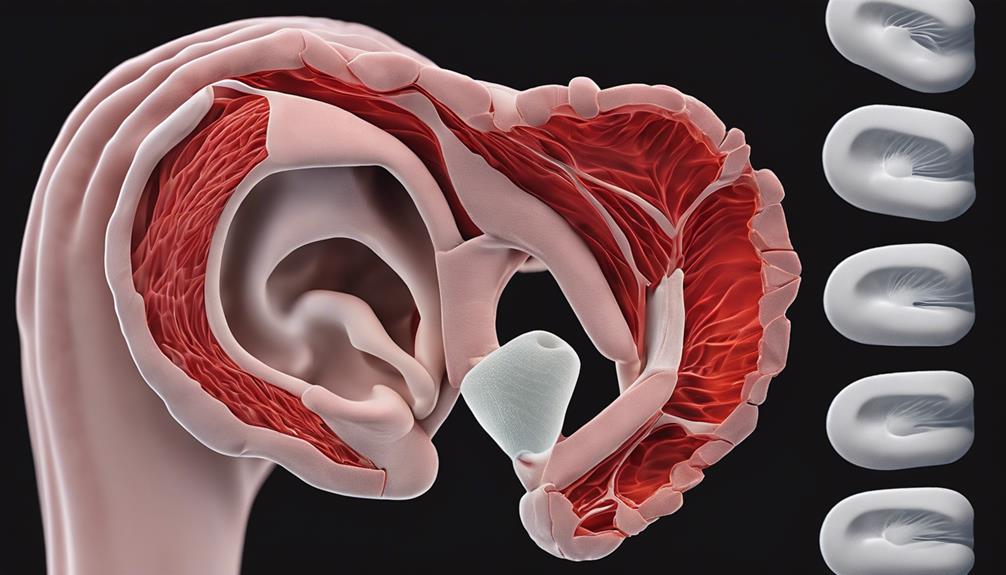
How Does Inflammation Cause Hearing Loss?
Inflammation, a hallmark of rheumatoid arthritis, damages inner ear structures, leading to hearing loss. The inflammatory process impacts the auditory nerve, cochlea, and blood flow, contributing to impairment.
Overproduction of antibodies and antigens can harm inner ear cells, further complicating hearing. This inflammatory response can disrupt sound transmission in the ear, exacerbating hearing difficulties.
Understanding these mechanisms is crucial in managing rheumatoid arthritis-related hearing loss.
Does Rheumatoid Arthritis Qualify for Disability?
Yes, rheumatoid arthritis can qualify for disability benefits if it significantly affects your ability to work. The severity of symptoms, functional limitations, and medical evidence are crucial factors in the determination process.
Meeting the Social Security Administration's criteria for disability due to rheumatoid arthritis can provide essential financial support. It's important to have documentation from healthcare providers detailing how rheumatoid arthritis impacts daily activities to support disability claims.
Conclusion
In conclusion, managing rheumatoid arthritis and its impact on hearing is crucial for overall well-being. Like a symphony, our health requires harmony and balance to function at its best.
By understanding the types of hearing loss associated with RA, being aware of the link between the two conditions, and utilizing early detection and management strategies, we can work towards maintaining optimal hearing health and quality of life.










